Stopping oxycodone after regular use can trigger a cascade of uncomfortable physical and psychological symptoms that many people find overwhelming.
Acute withdrawal from immediate-release oxycodone typically begins within 8–24 hours of the last dose, peaks around days 2–3, and resolves within 7–10 days, though extended-release formulations delay onset to 12–48 hours and can prolong symptoms to 10–20 days.
This article explains what to expect during oxycodone withdrawal, how long detox takes, which factors influence severity, and why evidence-based medical support, especially medications for opioid use disorder, dramatically improves safety and outcomes compared to detox alone.
What is Oxycodone Withdrawal?
Oxycodone is a semisynthetic opioid that binds strongly to μ-opioid receptors in the brain and body. When you take oxycodone regularly for more than a few days, your nervous system adapts to its presence.
Physical dependence can develop quickly, and when the drug is reduced or stopped, your body reacts with withdrawal symptoms that reflect the sudden absence of opioid activity at those receptors.
Withdrawal is not the same as addiction, though the two often overlap. Anyone who has taken oxycodone consistently, whether for legitimate pain management or misuse, can experience withdrawal when stopping.
The severity and duration depend on dose, formulation, length of use, and individual factors like metabolism and co-occurring conditions.
Common Oxycodone Withdrawal Symptoms
Oxycodone withdrawal produces a predictable cluster of autonomic, gastrointestinal, and neuropsychiatric symptoms.
While rarely life-threatening in otherwise healthy adults, the discomfort can be intense enough to derail recovery efforts without proper support.
Physical Symptoms
- Sweating and chills
- Rapid heartbeat and elevated blood pressure
- Dilated pupils
- Runny nose and watery eyes
- Muscle aches and joint pain
- Abdominal cramping
- Nausea, vomiting, and diarrhea
- Restlessness and tremors
Psychological Symptoms
- Anxiety and irritability
- Insomnia and sleep disturbance
- Dysphoria and low mood
- Difficulty concentrating
- Intense cravings for opioids
Clinicians often use the Clinical Opiate Withdrawal Scale (COWS) to quantify severity and guide treatment decisions.
Higher COWS scores indicate more severe withdrawal and typically warrant more intensive medical management.
How Long Does Oxycodone Detox Take?
The timeline for oxycodone withdrawal varies by formulation, dose, duration of use, and individual metabolism. Understanding these differences helps set realistic expectations and plan appropriate support.
Immediate-Release Oxycodone Timeline
For short-acting oxycodone products, withdrawal follows a relatively rapid course:
- Hours 8–24: Early symptoms emerge, yawning, watery eyes, runny nose, anxiety, restlessness, mild gastrointestinal discomfort, and early insomnia.
- Days 2–3: Peak severity, muscle aches, abdominal cramping, nausea, vomiting, diarrhea, rapid heartbeat, sweating, chills, significant insomnia, and heightened anxiety.
- Days 4–7: Physical symptoms gradually fade, though sleep remains poor and mood symptoms like dysphoria and anhedonia persist.
- Days 7–10: Most acute physical symptoms resolve, but psychological symptoms and cravings can linger.
Extended-Release Oxycodone Timeline
Extended-release formulations like OxyContin have longer half-lives and delayed withdrawal onset:
- Hours 12–48 (up to 72): Onset is delayed compared to immediate-release; prodromal symptoms slowly emerge.
- Days 3–4: Peak withdrawal intensity, often with prolonged gastrointestinal and autonomic symptoms.
- Days 5–14 (sometimes up to 20): Physical symptoms fade slowly; insomnia, anxiety, dysphoria, and cravings may intensify after the first week.
Protracted Withdrawal
After acute symptoms resolve, many people experience protracted or post-acute withdrawal syndrome (PAWS) for weeks to months.
Common features include persistent insomnia, mood instability, difficulty experiencing pleasure, heightened stress sensitivity, and ongoing cravings. Sleep disturbance is especially problematic because it drives craving and relapse risk.
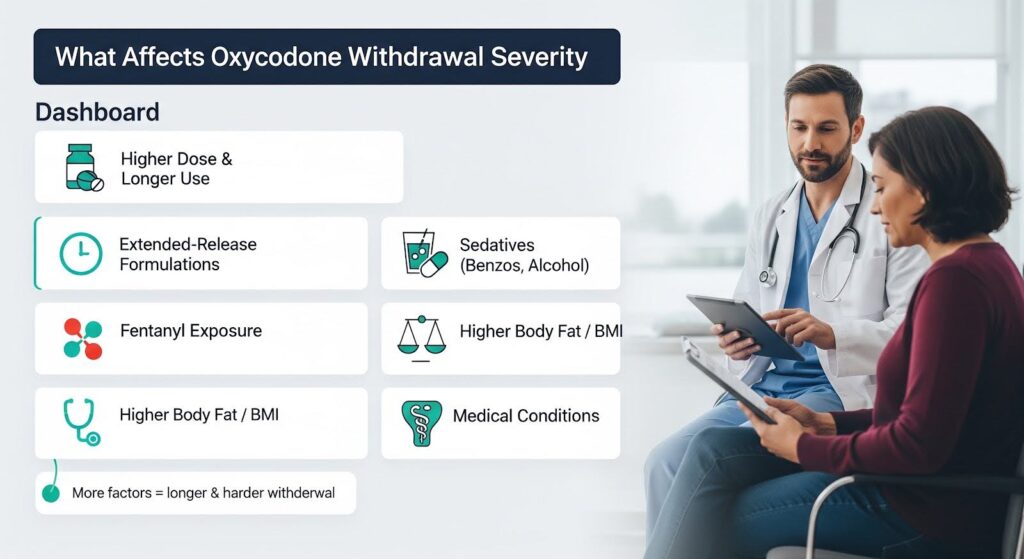
Factors That Influence Withdrawal Severity and Duration
Not everyone experiences oxycodone withdrawal the same way. Several factors determine how intense and prolonged your symptoms will be:
- Dose and duration: Higher daily doses and longer exposure increase symptom burden.
- Formulation: Extended-release products delay onset and extend the acute phase.
- Co-occurring sedative use: Benzodiazepines and other sedatives complicate withdrawal and raise overdose risk if re-use occurs.
- Fentanyl exposure: Illicitly manufactured fentanyls are now common in counterfeit “oxycodone” pills. Fentanyl’s high potency and lipophilicity prolong clearance and increase the risk of severe withdrawal when transitioning to medications like buprenorphine.
- Body mass index: Higher BMI is associated with longer fentanyl detectability and higher self-reported withdrawal severity.
- Medical comorbidities: Frail patients or those with cardiovascular, hepatic, or renal impairment may experience more severe physiologic stress during withdrawal.
Risks and Complications of Oxycodone Withdrawal
While opioid withdrawal itself is rarely fatal in healthy adults, complications can be serious, especially in vulnerable populations and institutional settings.
Medical Complications
Severe vomiting and diarrhea can lead to dehydration, electrolyte imbalances, and hemodynamic instability in frail or medically complex patients. Withdrawal also acts as a physiologic stressor that can destabilize underlying conditions.
Psychological and Relapse Risks
Untreated withdrawal drives intense cravings and relapse. Because tolerance drops during abstinence, returning to previous opioid doses, especially with fentanyl-contaminated supplies, carries high overdose risk. Sleep disturbance during and after withdrawal is a powerful predictor of relapse.
Institutional Risks: Hospitals and Jails
A thematic analysis of UK coroner reports found that opioid-related deaths during hospitalization or within 14 days of discharge often involved undertreated withdrawal and pain, zero-tolerance drug policies that pushed concealed use into unsafe spaces, and discharge to unstable settings.
Similar patterns occur in jails, where failure to treat withdrawal promptly can result in serious harm or death, and mortality risk spikes in the first two weeks after release.
Evidence-Based Management of Oxycodone Withdrawal
Safe, effective withdrawal management prioritizes individualized care, symptom relief, and transition to long-term treatment rather than detox as an endpoint.
Slow, Individualized Tapering
For patients on prescribed oxycodone for chronic pain, the CDC recommends slow tapers, starting around 10% of the original dose per week, or 10% per month for long-term therapy, with frequent reassessment and flexibility to pause or slow the taper if withdrawal symptoms impair function. Abrupt discontinuation is discouraged because it increases harm without benefit.
Symptomatic Support
Non-opioid medications can ease specific withdrawal symptoms:
- Alpha-2 agonists (clonidine or FDA-approved lofexidine) reduce autonomic hyperactivity like sweating, rapid heartbeat, and anxiety.
- Antiemetics and antidiarrheals manage gastrointestinal symptoms.
- NSAIDs and acetaminophen address muscle aches and pain.
- Sleep hygiene and behavioral interventions target insomnia, though severe cases may warrant careful pharmacologic support.
Medications for Opioid Use Disorder (MOUD)
For patients with opioid use disorder, buprenorphine or methadone is first-line care. These medications improve retention, reduce illicit opioid use, and lower overdose risk compared to detox alone.
Buprenorphine is typically started when objective withdrawal is present (COWS ≥ 8–13) to avoid precipitated withdrawal due to its high receptor affinity.
In the fentanyl era, standard buprenorphine induction can trigger severe precipitated withdrawal because residual fentanyl occupies receptors despite outward signs of withdrawal.
Low-dose buprenorphine initiation (microinduction) offers a safer alternative: microgram-to-low-milligram doses are introduced while continuing full-agonist opioids, then the full agonist is discontinued after sufficient partial-agonist coverage develops, often within 5–7 days.
Multicenter case series show this approach successfully transitions hospitalized patients on IV hydromorphone, oral oxycodone, or extended-release morphine to depot buprenorphine with minimal precipitated withdrawal.
Harm Reduction and Overdose Prevention
Every withdrawal management plan should include naloxone distribution, overdose education, and linkage to community supports. Given the prevalence of fentanyl in counterfeit pills, presuming fentanyl exposure and adjusting protocols accordingly is prudent.
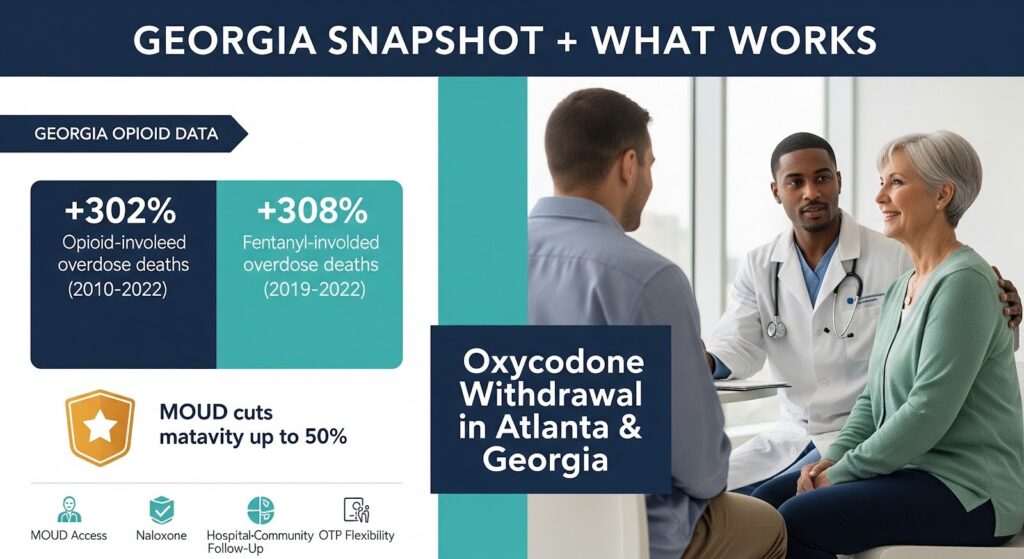
Oxycodone Withdrawal in Atlanta and Georgia
Georgia has experienced a 302% increase in opioid-involved overdose deaths from 2010 to 2022, driven largely by fentanyl. Fentanyl-involved deaths rose 308% from 2019 to 2022, underscoring the urgency of fentanyl-adapted withdrawal management and MOUD access.
Fulton County has appointed an Opioid Coordinator and collaborates with Grady Behavioral Health to provide MOUD at multiple sites.
County initiatives include drug disposal campaigns, school-based crisis text lines, and coordination of opioid abatement settlement funds. Public messaging recognizes that buprenorphine and methadone reduce mortality by up to 50%, a critical fact for discharge and re-entry planning.
For Atlanta-area residents, expanding hospital-to-community MOUD pathways, scaling naloxone distribution, and modernizing opioid treatment program (OTP) protocols to preserve methadone take-home flexibility are essential steps to reduce withdrawal-related harms and overdose deaths.
Practical Pathways for Safe Oxycodone Detox
Outpatient Taper Example
- Week 0: Establish goals, non-opioid analgesia plan, behavioral supports, sleep hygiene; prescribe naloxone; review benzodiazepine status.
- Weeks 1–4: Reduce total daily oxycodone by ~10% per week; adjust more slowly if symptoms impede function.
- Weeks 5–8+: Continue 10% decrements; when at very low doses, extend dosing intervals; stop when dosing is less than daily.
- At any point: Offer transition to MOUD if pain control, function, or withdrawal burden is problematic.
Inpatient Microinduction Pathway
- Day 0–1: Continue current full-agonist regimen for pain; initiate microdoses of buprenorphine per hospital protocol.
- Day 2–5: Gradually increase buprenorphine while maintaining full-agonist dosing; monitor COWS twice daily.
- Day 5–7: Achieve therapeutic buprenorphine dose; discontinue full agonists or administer depot buprenorphine with post-dose monitoring.
- Discharge: Provide follow-up MOUD appointment within 3–7 days; reconcile analgesia; ensure naloxone and harm-reduction supplies.
Why Detox Alone is Not Enough?
Focusing solely on “how long detox takes” risks trivializing the real determinants of success. Withdrawal timelines matter, but outcomes improve most when care aligns with neurobiology: using MOUD to stabilize physiology, tapering slowly and flexibly for chronic pain patients, addressing sleep explicitly to reduce craving and relapse, and embedding relapse-prevention skills like mindfulness-based approaches.
Detox done well is less about counting days and more about compassionate, evidence-based care that supports long-term recovery.
When to Seek Professional Help?
You should seek professional support for oxycodone withdrawal if you:
- Have been using oxycodone regularly for more than a few days
- Experience severe withdrawal symptoms that interfere with daily function
- Have co-occurring medical or psychiatric conditions
- Have a history of relapse after previous detox attempts
- Are using other substances, especially benzodiazepines or alcohol
- Suspect fentanyl exposure in your opioid supply
Medical supervision improves safety, comfort, and the likelihood of successful transition to long-term treatment.
Conclusion
Oxycodone withdrawal follows a predictable timeline, typically 7–10 days for immediate-release formulations and 10–20 days for extended-release products, but individual experiences vary widely based on dose, duration, formulation, co-occurring conditions, and fentanyl exposure.
While acute physical symptoms resolve within days to weeks, protracted psychological symptoms and sleep disturbance can persist for months and drive relapse risk.
The evidence is clear: slow, individualized tapers minimize withdrawal severity; medications for opioid use disorder improve retention and reduce overdose risk far better than detox alone; and fentanyl-era realities demand adapted protocols like microinduction to safely transition patients to buprenorphine.
Hospital and jail systems that treat withdrawal proactively, provide MOUD, and avoid punitive policies save lives.
If you or someone you care about is facing oxycodone withdrawal, compassionate, evidence-based support is available.
Reach out to Thoroughbred’s addiction counseling professionals who can guide you through safe detox and into lasting recovery.