Many people wonder if they can safely manage anxiety and muscle spasms by combining these medications.
You should generally avoid taking cyclobenzaprine and xanax together because they cause additive central nervous system depression, increasing the risk of falls and confusion especially in older adults.
This article explains the specific side effects and safety guidelines you need to know.
How Often Are Cyclobenzaprine and Xanax Taken Together?
Direct national estimates of how often people fill prescriptions for both cyclobenzaprine and alprazolam at the same time are not available in public datasets.
The National Survey on Drug Use and Health measures self‑reported substance use by class but is not designed to track specific drug‑pair concurrency.
Published prescription drug monitoring program reports have focused more on opioid–benzodiazepine combinations and the “Holy Trinity” of opioids, benzodiazepines, and carisoprodol rather than cyclobenzaprine–alprazolam pairs.
However, nationally representative emergency department surveillance from 2016 to 2017 provides the best proxy for harmful co‑exposure.
Among ED visits attributed to adverse events involving benzodiazepines, skeletal muscle relaxants were co‑involved in approximately 2.8% of nonmedical‑use visits, 4.1% of self‑harm visits, and 5.1% of therapeutic‑use visits.
Because cyclobenzaprine is one of the most commonly prescribed and misused muscle relaxants in the United States, it likely contributes a substantial fraction of these co‑exposures, though the surveillance system does not break down individual drugs within the muscle relaxant category.
This pattern suggests that while benzodiazepine–muscle relaxant co‑use is less common than opioid–benzodiazepine concurrency, it is present and clinically meaningful in harm‑related encounters.
The true outpatient co‑prescription rate is probably higher than the ED co‑involvement figure, since not all concurrent use leads to emergency visits, but it remains lower than the well‑documented prevalence of opioid–benzodiazepine overlap.
Risks of Taking Cyclobenzaprine and Xanax Together
Combining these two drugs creates a “double hit” to your central nervous system (CNS). Both medications work by slowing down brain activity, but they do so in different ways.
When you use them at the same time, the sedative effects do not just add up; they often multiply. This can lead to profound drowsiness, poor coordination, and an inability to think clearly.
National safety data highlights this danger. Emergency department surveillance shows that skeletal muscle relaxants are involved in approximately 3% to 5% of visits related to benzodiazepine harms.
While this might seem like a small number, it represents a significant group of patients who experienced adverse events severe enough to require emergency care.
The primary risk is that your body forgets to breathe properly or you become too sedated to function.
The FDA labeling for cyclobenzaprine warns that it may enhance the impairment caused by other CNS depressants.
This means that a standard dose of Xanax (alprazolam) might feel much stronger than usual if you are also taking a muscle relaxer.
Common Side Effects of This Combination
When you take xanax and cyclobenzaprine together, you will likely experience physical and mental side effects that impact your daily life.
The most immediate feeling is usually heavy fatigue. You might feel like you cannot keep your eyes open or that your limbs are heavy.
Beyond sleepiness, the combination can cause:
- Severe drowsiness: You may sleep for long periods or struggle to wake up.
- Dizziness and loss of balance: This increases the chance of stumbling or falling.
- Mental confusion: You might have trouble focusing, remembering things, or making decisions.
- Dry mouth and constipation: These are common anticholinergic effects of cyclobenzaprine.
- Psychomotor impairment: Your reaction times slow down, making driving dangerous.
These effects are unpredictable. Even if you have taken each drug separately without issues, the combination can catch you off guard.
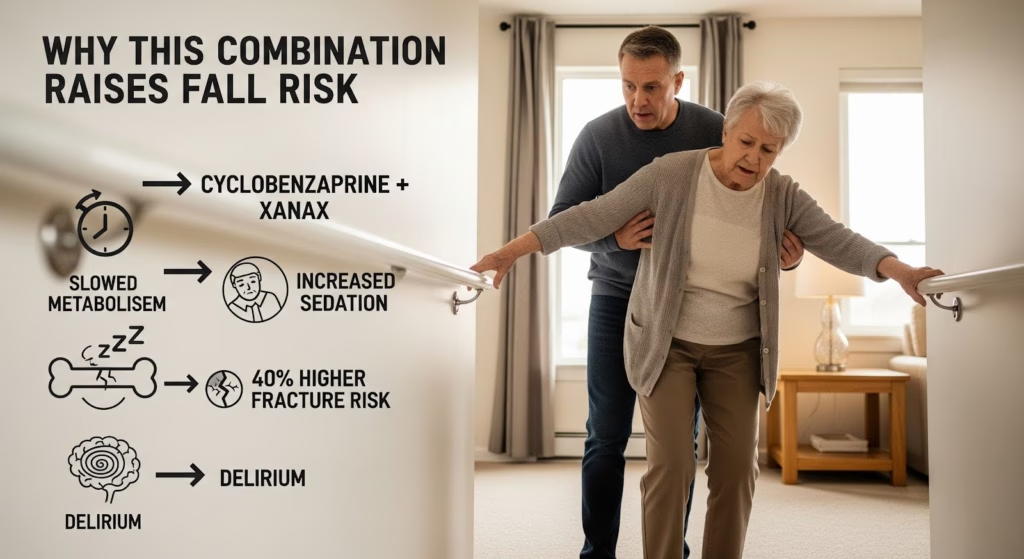
Why Older Adults Should Avoid Cyclobenzaprine and Xanax?
The risks of this combination are much higher for people over age 65. As we age, our bodies process drugs more slowly, meaning the medication stays in the system longer. Older adults are also more sensitive to the side effects of sedatives.
Medical guidelines are clear on this issue. The AGS Beers Criteria advises that older adults avoid benzodiazepines like Xanax and muscle relaxants like cyclobenzaprine.
Using them together is considered a high-risk practice because it dramatically increases the likelihood of delirium and falls.
Falls are a major health threat for seniors. Research indicates that using skeletal muscle relaxants is associated with a 40 percent increase in fracture risk.
When you add a benzodiazepine to the mix, that risk climbs even higher. For this reason, doctors rarely prescribe this pairing to older patients.
The Danger of Adding Alcohol or Opioids
The safety profile gets much worse if you add a third depressant, such as alcohol or opioid pain medication. Alcohol is frequently involved in medication-related emergencies.
In fact, alcohol was involved in over 20 percent of deaths related to benzodiazepines.
Alcohol acts as a fuel for the sedation caused by cyclobenzaprine and Xanax. It does not take much alcohol to turn a manageable side effect into a medical emergency, such as respiratory arrest.
Similarly, adding opioids (like hydrocodone or oxycodone) creates a dangerous “triple threat.” The CDC guidelines specifically warn clinicians to be cautious when prescribing opioids with other CNS depressants.
The combined weight of these drugs can stop your breathing while you sleep. If you are taking an opioid, you should generally not take cyclobenzaprine and xanax together.
Safer Alternatives for Pain and Anxiety
Because of the risks, experts recommend trying other treatments first. For acute back pain or muscle spasms, non-drug therapies often work better than sedatives.
Physical therapy, heat packs, and stretching can relieve muscle tightness without making you drowsy.
For anxiety, doctors may suggest non-sedating options. Cognitive behavioral therapy (CBT) is highly effective for managing anxiety disorders.
If medication is needed, antidepressants like SSRIs are often preferred over benzodiazepines for long-term treatment because they do not carry the same risk of dependence or sedation.
If you must take a muscle relaxant, your doctor might prescribe a very short course (less than two weeks) and advise you to stop taking Xanax during that time.
Always be honest with your healthcare provider about all the substances you use, including alcohol, so they can keep you safe.

Why Does It Matter?
Understanding the dangers of mixing these drugs can prevent serious injuries. A simple fall caused by dizziness can lead to a broken hip or a hospital stay, especially if you are older.
By respecting the power of these medications and avoiding the combination, you protect your brain and body from unnecessary harm.
If you or a loved one are struggling to stop using sedatives or need help managing co-occurring anxiety and substance use, Thoroughbred’s team offers a compassionate medical detox program to help you recover safely.