Stopping cocaine after heavy use triggers a withdrawal syndrome that can feel overwhelming.
The acute phase typically lasts one to two weeks, with fatigue, intense cravings, and mood swings peaking in the first few days. Many people experience lingering symptoms like sleep trouble and depression for two to three months.
This article explains what to expect during cocaine detox, how long withdrawal lasts, which symptoms require medical attention, and how to reduce the risk of relapse and overdose in today’s fentanyl-contaminated drug supply.
What Happens During Cocaine Withdrawal?
Cocaine withdrawal is dominated by psychological and sleep-related symptoms rather than the dangerous physical instability seen with alcohol or benzodiazepine withdrawal.
When you stop using cocaine, your brain’s dopamine system, which cocaine has overstimulated, needs time to recalibrate. This neurobiological reset produces a cluster of symptoms that evolve over weeks to months.
The most common withdrawal symptoms include intense cravings, severe fatigue, depression or anhedonia (inability to feel pleasure), anxiety and irritability, insomnia or excessive sleeping, vivid unpleasant dreams, slowed thinking, increased appetite, and occasional paranoia or hallucinations in heavy users.
These symptoms reflect persistent changes across neurotransmitter systems and brain circuits that do not reverse instantly after cessation.
Women who primarily smoke crack cocaine may experience more severe withdrawal, especially if they also use cannabis.
A longitudinal study of women with cocaine use disorder found that recent cannabis use was associated with higher withdrawal and depressive symptom severity during early abstinence, and that long-term cannabis abuse predicted greater rehospitalization risk over two and a half years.
How Long Does Cocaine Detox Take?
The answer depends on what you mean by detox. Medical stabilization of acute withdrawal typically takes about one week, but clinically meaningful symptoms often persist for two to four weeks, and some people experience protracted withdrawal lasting months.
Acute Phase: 24 Hours to Two Weeks
The first 24 to 72 hours bring peak intensity, especially for people who smoke crack. You may feel crushing fatigue, profound sadness, and overwhelming cravings.
A review of psychostimulant withdrawal concluded that acute symptoms generally improve within four to seven days, though mood and sleep disturbances often extend into the second week.
Early Protracted Phase: Weeks Two to Four
By the second week, the worst physical exhaustion usually lifts, but residual anxiety, depression, fragmented sleep, low motivation, and episodic cravings remain common.
Many treatment programs measure outcomes over eight to sixteen weeks, reflecting the realistic timeline for substantial symptom relief.
Late Protracted Withdrawal: One to Three Months or Longer
Post-acute withdrawal syndrome (PAWS) can include mood swings, anhedonia, ongoing sleep disruption, stress sensitivity, and cue-triggered cravings. Objective sleep studies show that sleep architecture disturbances improve gradually but incompletely over months, with large individual variation.
A study of women completing three weeks of inpatient detox found that significant withdrawal symptoms often persisted at discharge, underscoring that a standard two to three week detox does not guarantee symptom resolution for everyone.
| Phase | Typical Time Frame | Dominant Symptoms |
|---|---|---|
| Acute | 24–72 hours peak, up to 1–2 weeks | Intense craving, severe fatigue, depression, anxiety, insomnia or hypersomnia, vivid dreams |
| Early protracted | Weeks 2–4 | Residual anxiety and depression, sleep fragmentation, low motivation, episodic cravings |
| Late protracted (PAWS) | 1–3+ months | Mood lability, anhedonia, sleep disruption, stress reactivity, cue-triggered cravings |
Cocaine Detox Symptoms and Warning Signs
Most cocaine withdrawal symptoms are uncomfortable but not medically dangerous. However, certain red flags require immediate attention.
Severe Depression and Suicidality
A subset of people experience profound depression with suicidal thoughts during early withdrawal. Pooled estimates among cocaine users in treatment show very high rates of suicidal ideation and attempts.
Routine suicide screening using validated tools is essential during the first week of detox, and anyone expressing suicidal thoughts needs urgent psychiatric evaluation and safety planning.
Psychosis-Like Features
Heavy crack use, especially combined with sleep deprivation, can trigger transient paranoia, hallucinations, and agitation.
These symptoms require careful assessment to distinguish acute intoxication, withdrawal, polysubstance effects, or an underlying psychotic disorder. Environmental safety and, when necessary, short-term antipsychotic medication may be needed.
Cardiovascular Concerns
While cardiovascular complications are more common during active cocaine use, people with chronic cocaine use often have underlying heart disease.
If you experience chest pain, palpitations, or severe high blood pressure during detox, seek medical evaluation promptly.
Skin Lesions and Unexplained Illness
Levamisole, a common cocaine adulterant, can cause a serious condition called thrombotic vasculopathy, marked by skin necrosis (especially on the ears), joint pain, and dangerously low white blood cell counts.
A case review of levamisole-adulterated cocaine emphasized that diagnosis relies on exposure history and skin biopsy rather than blood tests alone. If you develop unusual skin lesions or feel severely ill during detox, tell your medical team immediately.
Cocaine Withdrawal Death Rate and Overdose Risk
Cocaine withdrawal itself is rarely life-threatening from a physiologic standpoint. The real danger lies in what happens after detox: relapse into a drug supply contaminated with fentanyl and other potent opioids.
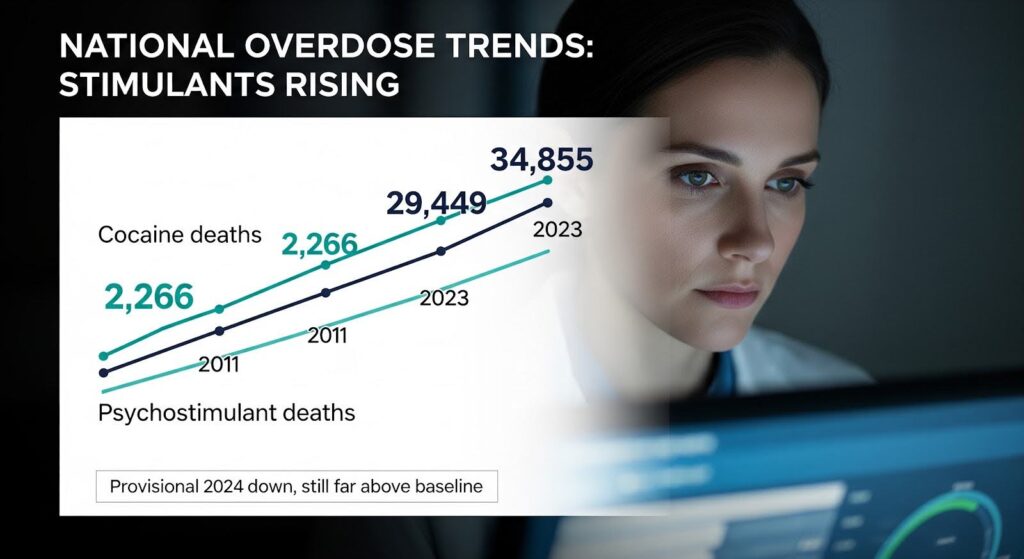
National Overdose Trends
Stimulant-involved overdose deaths have surged since 2011. CDC surveillance data show that cocaine deaths rose from 4,681 in 2011 to 29,449 in 2023, and psychostimulant deaths (mostly methamphetamine) increased from 2,266 to 34,855 over the same period.
Although provisional 2024 data show declines, levels remain far above 2011 baselines. Among 309,274 overdose deaths from January 2021 through June 2024, 59 percent involved stimulants, with 30 percent involving cocaine specifically.
The primary driver of these increases is opioid co-involvement. Illicitly manufactured fentanyls have extensively infiltrated cocaine and methamphetamine supplies, making relapse after stimulant detox unusually lethal.
Some people who identify as stimulant-only users unknowingly consume opioid-adulterated drugs; emergency departments have documented “stimulant overdoses” reversing with naloxone, direct evidence of hidden fentanyl exposure.
Cocaine Withdrawal Death Rate in Atlanta, Georgia
Georgia Department of Public Health surveillance aligns with national patterns. In March 2022, Georgia DPH issued an alert following increased overdoses from fentanyl-laced cocaine, methamphetamine, and counterfeit pills, documenting at least 66 emergency department visits in a six-week period.
Metro Atlanta county data reveal geographic and racial disparities. DeKalb County saw total overdose deaths rise from 142 in 2020 to 217 in 2023 before declining to 203 in 2024, with cocaine–fentanyl co-involvement common.
Suburban counties including Cobb, Gwinnett, Cherokee, Henry, and Clayton experienced peaks in 2022 followed by stabilization or decline in 2023 and 2024, attributed to expanded naloxone distribution and early fentanyl test strip integration.
However, the polysubstance environment remains entrenched, complicated by emerging adulterants like xylazine and nitazenes.
Regional analyses highlight that cocaine–fentanyl co-involvement risk is elevated in Black communities, particularly in southern and eastern Gwinnett, south Cobb, and Clayton County. These patterns underscore the need for culturally tailored harm reduction and treatment access.
Loss of Tolerance After Detox
Even a brief period of abstinence reduces your tolerance to both stimulants and opioids. If you relapse after detox, the same dose that you previously used can be fatal, especially if it contains fentanyl.
This dynamic is well documented in opioid users post-detox and applies equally in polysubstance environments where stimulant users may inadvertently undergo an opioid tolerance reset.
Who Should Consider Inpatient Detox?
Outpatient detox works well for many people with reliable support and no severe psychiatric instability. However, inpatient or residential detox is recommended when:
- You have severe withdrawal symptoms, including high scores on validated scales like the Cocaine Selective Severity Assessment (CSSA), profound depression, or suicidal thoughts.
- You use multiple substances, especially if opioid involvement is likely (intentional or unintended).
- You have significant psychiatric conditions such as major depression, PTSD, bipolar disorder, or a history of psychosis.
- You have medical issues requiring monitoring, such as unstable cardiovascular disease or pregnancy.
- You have repeatedly tried to quit in outpatient settings without success, or your home environment is filled with triggers.
A study of women with cocaine use disorder emphasized that early identification of severe or persistent withdrawal is clinically important because it predicts poorer long-term outcomes.
Standardized assessment at intake helps clinicians decide on the right level of care and plan extended support for high-severity patients.
Managing Cocaine Withdrawal Symptoms
There is no FDA-approved medication specifically for cocaine withdrawal. Management relies on symptomatic treatment, behavioral therapies, and close monitoring.
Symptom-Targeted Medications
Clinicians commonly use off-label medications to address specific symptoms:
- Anxiety and autonomic arousal: Clonidine or propranolol can reduce anxiety, rapid heart rate, and blood pressure spikes. Providers monitor for low blood pressure and avoid propranolol in people with asthma or very slow heart rates.
- Insomnia: Trazodone or low-dose quetiapine may be prescribed short-term. Sleep hygiene and behavioral sleep interventions are first-line, given that sleep architecture disturbances persist for months and contribute to mood instability and relapse risk.
- Agitation or psychosis-like features: Antipsychotics such as haloperidol or atypical agents may be used cautiously, with careful assessment to rule out intoxication or a primary psychotic disorder.
- Neuropathic discomfort and anxiety: Gabapentin is sometimes used off-label, though providers monitor for misuse potential.
- Depression: If major depression is diagnosed, SSRIs or SNRIs may be started, with close monitoring for suicidality and attention to distinguishing substance-induced depression from independent mood disorders.
These medications are symptomatic supports rather than anti-craving agents. The strongest evidence for promoting abstinence and retention comes from behavioral therapies.
Behavioral Therapies
Contingency management (CM) consistently demonstrates the best outcomes for stimulant use disorder. CM provides tangible rewards (vouchers, prizes) for verified abstinence, reinforcing positive behavior change.
When paired with cognitive behavioral therapy (CBT) or community reinforcement approaches, CM helps people identify triggers, develop coping skills, and build a recovery-supportive lifestyle.
Polysubstance and Opioid Use Disorder Integration
For patients with concurrent or suspected opioid use, initiating medications for opioid use disorder (buprenorphine or methadone) is critical to reduce overdose and relapse risk.
This is essential even in “stimulant-primary” populations due to fentanyl contamination dynamics. Reviews of opioid withdrawal management in the fentanyl era emphasize low-barrier access to these medications.
Reducing Overdose Risk After Detox
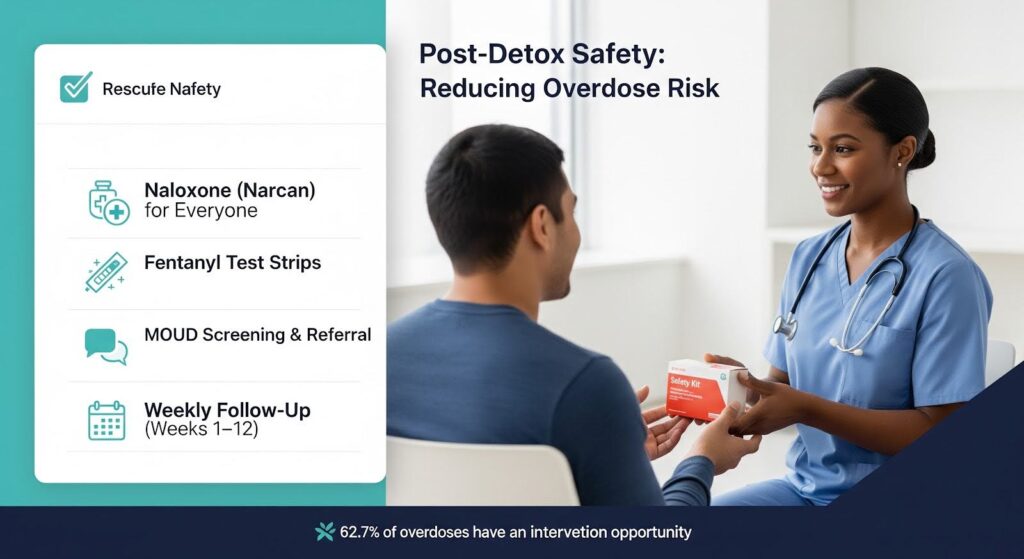
The period immediately after detox is the highest-risk window for fatal overdose. Comprehensive discharge planning should include:
- Naloxone for everyone: All patients and their household members should receive naloxone (Narcan) and training on overdose recognition and response, regardless of reported opioid use. Pre-fentanyl-era surveillance documented that 62.7 percent of overdose deaths had at least one potential opportunity for intervention, signaling practical room for prevention.
- Fentanyl test strips: Provide test strips with clear instructions tailored to stimulant use patterns. While not foolproof, they can detect fentanyl in cocaine and methamphetamine samples and prompt safer use decisions.
- Medications for opioid use disorder: Screen all stimulant detox patients for opioid use disorder and offer immediate initiation or referral to buprenorphine or methadone for any positive screen or suspected exposure.
- Frequent early follow-up: Schedule weekly contacts (in person or telehealth) during the first eight to twelve weeks post-detox to reinforce contingency management and CBT, monitor sleep and mood, and reassess relapse risk.
- Culturally tailored linkages: In metro Atlanta, connect patients from high-burden areas to trusted community resources distributing naloxone and test strips, and coordinate with county-level harm reduction initiatives.
Predictors of Severe or Prolonged Withdrawal
Certain factors increase the likelihood of intense or long-lasting withdrawal symptoms:
- Early severity: Higher scores on the Cocaine Selective Severity Assessment (CSSA) at treatment entry predict worse abstinence outcomes and justify extended support.
- Depressive symptom burden: Greater depression correlates with heightened withdrawal severity and poorer trajectories.
- Recent and historical cannabis use: Among women with smoked cocaine use disorder, recent cannabis consumption associates with greater withdrawal and depressive severity during early abstinence, and long-term cannabis abuse predicts higher rehospitalization risk.
- Polysubstance co-use: Frequent upper-downer co-use (stimulants and opioids) can mask or distort classic withdrawal syndromes and increase relapse risk for either drug class.
- Sleep disturbance: Severe insomnia or fragmented sleep during detox may signal the need for early sleep-focused interventions, as persisting sleep abnormalities correlate with mood and relapse risk.
- Psychosocial factors: Unstable housing, trauma history, lack of social support, and co-occurring mental health conditions all intensify withdrawal experiences and complicate care.
Incorporating these predictors into early triage improves risk stratification and helps allocate resources effectively.
A Realistic Timeline for Recovery
For most people, the acute medical stabilization phase of cocaine detox lasts about one week. However, a realistic care plan should anticipate two to four weeks for major symptom improvement and commit to at least eight to twelve weeks of structured support to address persistent symptoms, relapse risk, and safety needs.
Days 0–7: Expect peak fatigue, cravings, and mood swings. Daily contact, suicide screening, sleep hygiene coaching, and initiation of contingency management are essential. If you use alcohol with cocaine, cardiovascular monitoring may be needed due to cocaethylene formation.
Weeks 2–4: Acute exhaustion typically lifts, but residual anxiety, depression, sleep fragmentation, and episodic cravings remain common. Continue contingency management and CBT, focusing on trigger mapping and coping skills. Monitor mood closely and evaluate for major depressive disorder or anxiety disorders if symptoms are severe or persistent.
Months 2–3 and beyond: Protracted withdrawal symptoms can fluctuate for months. Maintain longer-term supports such as community reinforcement approaches, peer recovery groups, and relapse prevention planning. Address co-occurring disorders and refresh skills before high-risk events.
When to Seek Help?
You should seek professional help for cocaine detox if:
- You have tried to quit on your own and experienced severe depression, suicidal thoughts, or intense cravings that led to relapse.
- You use cocaine with other substances, especially opioids or alcohol.
- You have a history of mental health conditions such as depression, anxiety, PTSD, or bipolar disorder.
- You have medical issues like heart disease or high blood pressure.
- Your home environment is unstable or filled with triggers.
Professional detox programs provide medical monitoring, symptom management, suicide risk assessment, and a structured transition to ongoing treatment.
Inpatient settings offer 24-hour support and a protected environment to break cycles and plan aftercare.
Moving Forward
Cocaine withdrawal is a neurobiologically mediated, protracted syndrome with individually variable trajectories.
The acute phase typically resolves within one to two weeks, but clinically meaningful symptoms often extend for two to four weeks, and some people experience post-acute withdrawal lasting months. The most consequential mortality threat is not withdrawal physiology itself but relapse into a fentanyl-saturated drug supply.
Evidence-informed detox in 2026 must bundle naloxone and fentanyl test strips for all stimulant users, integrate on-demand medications for opioid use disorder for concurrent or suspected opioid use, and deliver contingency management and cognitive behavioral therapy with sleep-focused supports.
Early identification of severe withdrawal, attention to co-use modifiers like cannabis, and proactive mood and suicide risk management improve outcomes.
If you or someone you care about is struggling with cocaine use, know that effective treatment exists. With the right support, medical care, and behavioral therapies, recovery is possible.
If you’re ready to take the next step, explore Thoroughbred Wellness and Recovery’s detox programs to learn how personalized, compassionate care can guide you toward lasting freedom.