If you’re considering Dialectical Behavior Therapy, you’re probably wondering what it will cost.
DBT therapy typically ranges from $75 to $170 per individual session and $60 to $100 per group skills class, with comprehensive programs often running $185 to $300 per week depending on your location and provider credentials.
This article breaks down the real costs you can expect, explains what drives DBT pricing higher or lower, and shows you how insurance and payment options can make this evidence‑based treatment more accessible.
What Makes DBT Different From Regular Therapy?
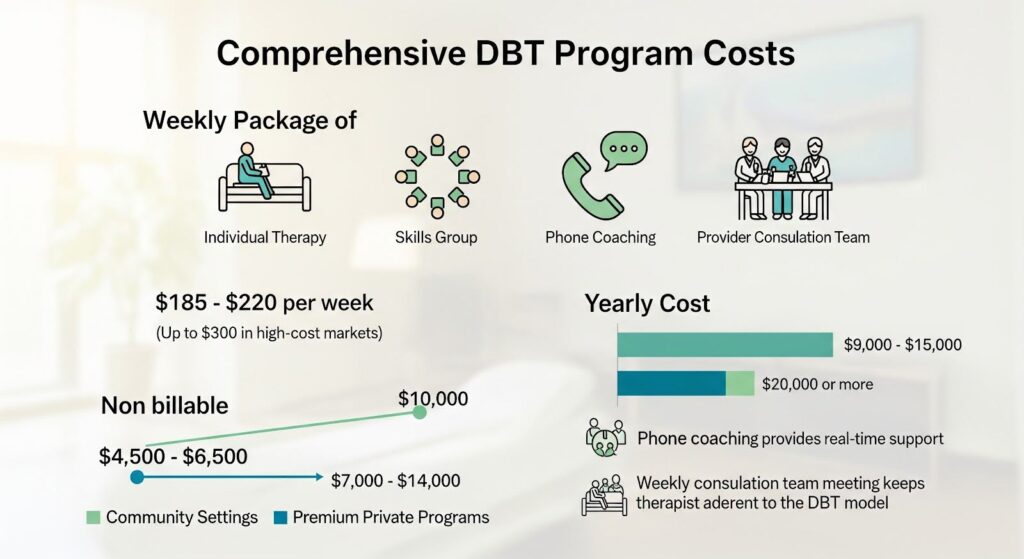
Dialectical Behavior Therapy is not a single weekly appointment. Comprehensive DBT combines four distinct components: weekly individual therapy sessions lasting 50 to 60 minutes, weekly skills training groups that run 2 to 2.5 hours, between‑session phone coaching to help you apply skills in real time, and a provider consultation team that keeps your therapist supported and on track.
This integrated structure is what sets DBT apart from standard outpatient counseling and directly influences the total cost.
The skills training groups teach mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness over roughly 24 weeks, with many people completing two full cycles for a total of about one year. Because you’re receiving multiple hours of clinical contact each week plus access to coaching between sessions, the time commitment and cost exposure are higher than traditional once‑weekly psychotherapy.
How Much Individual DBT Sessions Cost?
Individual DBT therapy sessions in the United States commonly cost between $75 and $170 per hour when paying out of pocket. In high‑cost metropolitan areas like New York or Los Angeles, rates can climb to $200 or more per session, especially when working with doctoral‑level clinicians or certified DBT specialists.
When you use insurance, your out‑of‑pocket cost typically falls between $20 and $40 per session as a copay or coinsurance amount, depending on your plan’s benefit design. Medicare beneficiaries generally pay 20 percent of the Medicare‑approved amount after meeting their Part B deductible, which translates to roughly $30 per 60‑minute session in many localities.
Commercial insurance plans reimburse individual psychotherapy using standard CPT codes 90834 for 45‑minute sessions and 90837 for 60‑minute sessions.
National average allowed amounts for 90837 hover around $154, though actual rates vary widely by payer, state, and provider credentials. Telehealth sessions are now reimbursed at the same rate as in‑person visits by most insurers, expanding access without changing your cost share.
DBT Skills Group Pricing
DBT skills training groups are typically priced at $60 to $100 per session, with each session lasting 2 to 2.5 hours. Because group therapy spreads clinician time across multiple participants, the per‑client cost is lower than individual sessions even though two co‑leaders often facilitate the class.
Real‑world examples illustrate this range. HRC Behavioral Health in North Carolina charges $60 per session for virtual DBT skills classes on a self‑pay basis. Verdant Hope in Arizona bundles six‑week skills modules at $300 total, which works out to $50 per week.
Some programs in major metros charge closer to $100 per group session, reflecting higher overhead and dual‑facilitator staffing.
With insurance, group therapy copays often mirror individual session copays, typically $20 to $40 per session. However, coverage for group psychotherapy can vary by plan, so it’s important to verify that your insurer reimburses CPT code 90853 for group therapy and whether telehealth delivery is covered under the same terms.
Comprehensive DBT Program Costs
Many DBT programs bundle all four components into a weekly package that includes individual therapy, skills group, phone coaching access, and the provider consultation team.
These bundled programs commonly price at $185 to $220 per week, with some reaching $300 per week in high‑cost markets or when delivered by highly credentialed teams.
Bundled pricing helps cover the non‑billable elements of DBT that are clinically essential but not always reimbursed by insurance under standard outpatient codes. Phone coaching, for example, provides real‑time support when you’re facing a crisis or trying to apply a skill in the moment, but many insurers do not pay separately for between‑session contact.
The weekly consultation team meeting that keeps your therapist adherent to the DBT model is another program cost that is rarely billable to patients or payers.
Over six months, a bundled comprehensive DBT program can total roughly $4,500 to $6,500 at the lower end of the pricing spectrum and $7,000 to $14,000 at the higher end. A full year of treatment may range from $9,000 to $15,000 in community settings and climb toward $20,000 or more in premium private programs.
What Drives DBT Costs Higher or Lower?
Program Intensity and Staffing
The most significant cost driver is the multi‑modal structure itself. You’re receiving approximately 3.5 hours of clinical contact each week when you add individual therapy, group skills training, and periodic phone coaching.
Over six months, that totals roughly 91 hours of direct service, far exceeding the 26 hours you would accumulate in standard weekly therapy.
DBT skills groups are commonly led by two clinicians, which doubles the staffing cost compared to single‑leader groups. Louisiana Medicaid’s DBT billing guidance explicitly expects two co‑leaders for 120 to 150‑minute sessions and reimburses $177.68 per client per week for group skills training to support that model.
Programs must maintain adequate group enrollment to balance the cost of dual facilitators, which can be challenging in smaller markets.
Non‑Billable Components
Phone coaching and the provider consultation team are core to DBT fidelity but are often not separately reimbursed under traditional fee‑for‑service insurance. Programs either absorb these costs, risking financial strain and reduced capacity, or shift them to self‑pay bundles and enhanced program fees.
Some state Medicaid programs have addressed this gap by creating DBT‑specific enhanced rates that explicitly fund non‑visit time, improving program sustainability and fidelity.
Clinician Credentials and Certification
Provider credentials influence both reimbursement rates and self‑pay pricing. Psychologists and psychiatrists typically command higher fees than master’s‑level clinicians, and Medicare and commercial payers often pay differentially by license type.
DBT‑Linehan Board of Certification is the recognized independent credentialing body for DBT clinicians and programs, and certification fees total roughly $870 for individual clinicians across application, exam, and work product, plus $95 annually for maintenance.
While not required by most payers, certification signals quality and adherence to the evidence base, and some programs price certified providers at a premium.
Geographic and Market Factors
Location matters. Urban centers with higher wages and real estate costs tend to have higher DBT fees. Telehealth has expanded access across state lines where licensing allows, potentially giving you access to programs outside your immediate metro area at varying price points.
Rural and underserved areas may have fewer DBT providers, limiting competition and sometimes driving prices up or requiring longer waitlists for lower‑cost community programs.
Insurance Coverage and Reimbursement
Most insurance plans cover DBT under general outpatient mental health benefits rather than issuing a separate DBT‑specific policy. Clinicians bill standard psychotherapy codes—90834 or 90837 for individual sessions and 90853 for group therapy, and your plan adjudicates them like any other outpatient counseling.
Medicare covers psychotherapy in all settings and pays for telehealth at the same rate as in‑person visits, with beneficiaries owing 20 percent coinsurance after the Part B deductible. Commercial plans have largely aligned telehealth reimbursement with in‑person rates for behavioral health, though you should confirm your plan’s telehealth policies and any required modifiers or place‑of‑service codes.
A notable exception is Louisiana Medicaid, which uses DBT‑specific HCPCS codes H2021 for individual DBT and H2021‑HQ for group DBT, with explicit weekly rates of $200 per 60‑minute individual session and $177.68 per client for group skills training.
This approach directly funds the four‑modality model, including phone coaching and consultation team time, and represents a reimbursement design aligned with program fidelity.
When seeking coverage, verify whether your plan covers individual therapy, group therapy, and telehealth delivery. Ask about copays, coinsurance, deductibles, and any session limits.
If your insurer does not have in‑network DBT providers in your area, you may be able to request a single‑case agreement or out‑of‑network reimbursement, especially if you can document medical necessity and network inadequacy.
Skills‑Only Classes vs Comprehensive DBT
Many community programs offer standalone DBT skills classes that teach the four skill modules without the full individual therapy, phone coaching, and consultation team structure.
These classes are more affordable, often priced at $60 per session or bundled into four‑week workshops for around $250, and can be a practical entry point for people who want to learn DBT strategies without committing to the full program.
However, skills‑only formats are not equivalent to comprehensive DBT for high‑risk populations. A head‑to‑head trial comparing standard DBT, DBT skills training plus case management, and DBT individual therapy plus activities group found that the composition of treatment matters for outcomes.
For individuals with borderline personality disorder, chronic suicidality, or severe emotion dysregulation, the integrated model delivers the strongest evidence base.
Skills classes work well as adjuncts or for lower‑acuity needs, and many programs require participants to maintain an individual therapist elsewhere.
If you’re considering a skills‑only option to save money, discuss with a clinician whether it matches your clinical needs or whether comprehensive DBT is indicated.
Cost‑Effectiveness and Long‑Term Value
DBT is more expensive up front than routine outpatient therapy, but research consistently shows it can be cost‑effective or even cost‑saving over time.
A 2019 economic evaluation found DBT more expensive and more effective than treatment as usual in the short term, yet with a low incremental cost‑effectiveness ratio and a greater than 50 percent probability of being cost‑effective across scenarios.
The largest cost offsets come from reduced hospitalizations and emergency room visits. A 2024 trial in autistic adults with suicidal behaviors found a 64 percent likelihood that DBT was dominant, delivering more quality‑adjusted life years at lower total cost, from a healthcare perspective, with reduced hospital admissions driving the savings.
Adolescent DBT studies show higher outpatient costs offset by reductions in inpatient and ER use, resulting in cost neutrality or net savings at the system level within 12 months.
Behavioral Tech Institute’s synthesis reports that standard outpatient DBT reduces healthcare costs by nearly $20,000 per person compared to prior treatment, with most savings from decreased inpatient use.
For payers and families, this means the higher weekly therapy bill can be offset by avoiding a single hospitalization, making DBT economically rational when delivered with fidelity to high‑risk populations.

Practical Strategies to Reduce Out‑of‑Pocket Costs
- Verify insurance coverage early. Call your insurer to confirm coverage for individual psychotherapy (CPT 90834/90837), group therapy (CPT 90853), and telehealth delivery. Ask about copays, coinsurance, deductibles, and any session limits or prior authorization requirements.
- Prioritize group skills training. Because group therapy spreads clinician time across participants, the cost per therapeutic hour is lower than individual sessions. For some people, starting with a skills group while maintaining a separate individual therapist can be a more affordable path.
- Explore sliding‑scale and training programs. University training clinics and community mental health centers often offer DBT at reduced rates, with services delivered by supervised trainees. These programs can cut costs by 50 to 80 percent compared to private practices.
- Ask about bundled pricing and upfront discounts. Some programs offer discounts if you pay for six or twelve months in advance. Confirm refund policies before committing to a long‑term payment.
- Use out‑of‑network benefits and single‑case agreements. If your plan lacks in‑network DBT providers, request out‑of‑network reimbursement or a single‑case agreement. Document medical necessity and network inadequacy to strengthen your request.
- Leverage telehealth to expand options. Telehealth allows you to access DBT programs outside your immediate area, potentially at different price points. Verify that your insurer covers telehealth for psychotherapy and that the provider is licensed in your state.
Why Does This Matter?
Understanding DBT’s cost structure helps you make informed decisions about treatment. The higher weekly price reflects a more intensive, multi‑component model designed for people with complex needs, chronic suicidality, self‑harm, severe emotion dysregulation, and co‑occurring disorders.
When delivered with fidelity, DBT not only improves symptoms but also reduces the costly crises that drive emergency and inpatient use.
For payers and programs, aligning reimbursement with fidelity, through enhanced rates, bundled payments, or value‑based contracts, supports sustainable access to a treatment that delivers measurable outcomes and system‑level savings.
For individuals and families, knowing the typical price ranges, insurance mechanics, and cost‑reduction strategies empowers you to pursue the care you need without unnecessary financial strain.
If you or someone you care about is struggling with emotion dysregulation, self‑harm, or co‑occurring mental health and substance use challenges, comprehensive treatment that addresses both dimensions can make all the difference.
So, reach out to Thoroughbred Wellness and Recovery today to explore dual diagnosis treatment options that integrate evidence‑based therapies like DBT with personalized, compassionate support.