Georgia’s opioid crisis has shifted dramatically over the past decade, leaving families and policymakers wondering which substances pose the greatest threat today.
In 2025, prescription opioids such as oxycodone, hydrocodone, and methadone are responsible for more overdose deaths among Georgia residents than heroin, according to state surveillance data and the CDC’s State Unintentional Drug Overdose Reporting System.
This article explains how Georgia tracks these deaths, what the numbers reveal, and why understanding the difference matters for prevention and treatment.
How Georgia Defines and Tracks Opioid Overdose Deaths?
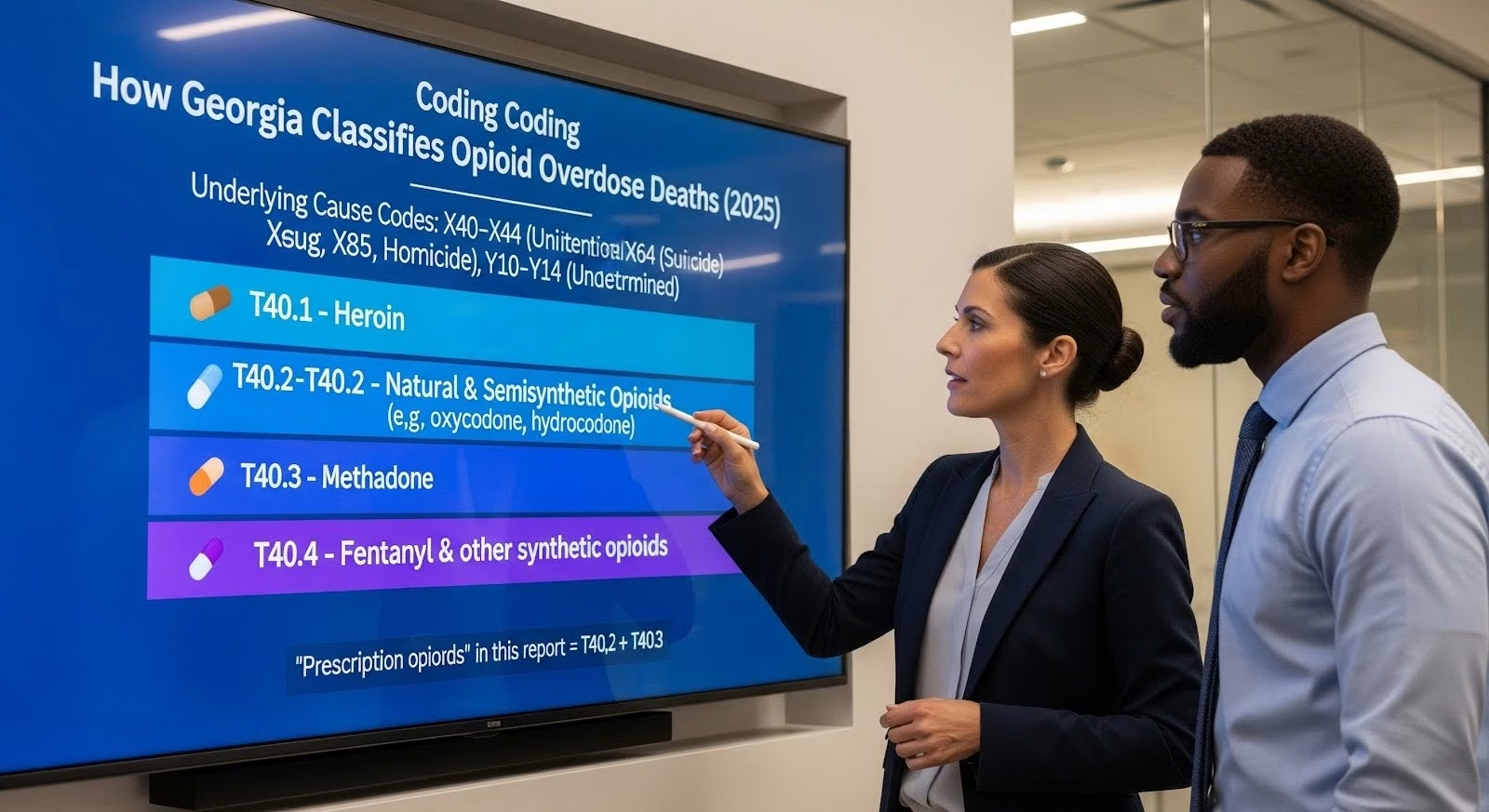
Georgia’s Department of Public Health uses a standardized coding system to classify overdose deaths.
Every fatal drug poisoning receives an underlying cause code (X40–X44 for unintentional, X60–X64 for suicide, X85 for homicide, or Y10–Y14 for undetermined intent).
Additional codes identify which substances were involved:
- T40.1 marks heroin involvement
- T40.2 captures natural and semisynthetic opioids like oxycodone, hydrocodone, and morphine
- T40.3 identifies methadone
- T40.4 covers synthetic opioids other than methadone, primarily fentanyl
For this comparison, “prescription opioids” means deaths involving T40.2 or T40.3, while “heroin” refers to T40.1. These categories can overlap because one death may list multiple substances.
The Georgia OASIS system tracks all counts by place of residence, not where the death occurred, ensuring accurate attribution to Georgia communities.
The 2025 Landscape: Prescription Opioids Lead Heroin in Fatal Involvement
When comparing head to head, prescription opioids appear on more Georgia death certificates than heroin in 2025.
This finding comes from SUDORS final data, which integrates death certificates, medical examiner reports, and full toxicology results for over 600 data points per case.
The system’s quality controls and state level specificity allow direct comparison of heroin versus prescription categories.
Several factors explain this pattern:
- Prescribing volume: Despite reductions from peak years, natural and semisynthetic opioids remain widely prescribed for pain in Georgia, sustaining exposure risk through both medical use and diversion.
- Methadone’s dual role: Methadone serves as both a pain medication and a treatment for opioid use disorder. Its separate tracking under T40.3 adds to the prescription opioid tally, and it carries overdose risk especially during dose adjustments or when combined with sedatives.
- Heroin market displacement: Illicitly manufactured fentanyl has largely replaced heroin in many drug markets since 2016, reducing heroin’s coded involvement even as overall opioid deaths remain high.
Why Fentanyl Changes Everything?
While prescription opioids exceed heroin in this comparison, both are overshadowed by fentanyl (T40.4). Fentanyl now dominates Georgia’s opioid mortality landscape, often appearing alongside other drugs in polysubstance deaths.
The CDC’s SUDORS dashboard shows that fentanyl contamination has spread beyond heroin into counterfeit pills and stimulants, altering risk profiles across all drug categories.
Understanding Polysubstance Involvement and Measurement Challenges
One death can count in multiple categories. A person who dies with both heroin and methadone in their system will appear in both the heroin and prescription opioid tallies.
This overlap is intentional in surveillance systems because it reflects the reality of polysubstance use and helps identify which combinations drive mortality.
Three measurement issues complicate direct comparisons:
- Heroin detection bias: Heroin metabolizes to morphine. If the unique heroin marker (6 monoacetylmorphine) is not detected and scene evidence is unclear, a heroin death may be coded as morphine only (T40.2), artificially lowering heroin counts and raising prescription opioid counts.
- Toxicology variation: Not all jurisdictions test for the same substances or use identical detection thresholds, though SUDORS integration of medical examiner narratives helps reduce this.
- Coding transitions: Nonfatal surveillance adopted new codes for fentanyl in 2020, but mortality coding retained the T40.4 category, so analysts must avoid conflating the two systems.
Despite these caveats, the directional finding holds: prescription opioids involve more Georgia deaths than heroin in 2025.
What Does This Means for Prevention and Treatment in Georgia?
The prescription opioid burden calls for targeted strategies that differ from heroin focused interventions:
Clinical and prescribing safeguards
- Use Georgia’s Prescription Drug Monitoring Program to identify risky combinations or high dose patterns before prescribing
- Follow CDC aligned opioid prescribing guidance, considering non opioid therapies and safe tapering when appropriate
- Ensure methadone safety through careful dosing, especially during treatment induction and care transitions
- Screen patients on high dose opioids for overdose risk and provide naloxone to them and their families

Expanding access to medications for opioid use disorder
Buprenorphine, methadone, and extended release naltrexone save lives. Georgia should scale access by co-locating these medications with primary care and behavioral health services, reducing barriers like transportation and stigma.
Post overdose linkage programs that connect hospital patients to treatment immediately after a nonfatal event are especially effective.
Harm reduction across all opioid types
Naloxone distribution, fentanyl test strips, and overdose education remain essential statewide. Even when prescription opioids are the primary exposure, fentanyl contamination risk exists through counterfeit pills. For people who use heroin, services should address fentanyl and emerging adulterants like xylazine.
Equity centered approaches
SUDORS demographic data reveal disparities by age, race, and geography. Prescription opioid deaths concentrate among older adults and in rural counties, while heroin historically affected younger urban populations. Tailoring interventions to these patterns, with culturally relevant messaging and community partnerships, improves outcomes.
How to Verify the 2025 Georgia Comparison Yourself?
Anyone can confirm this finding using public data:
- Visit the CDC SUDORS Dashboard and select the Final Data view (updated November 12, 2025).
- Filter for Georgia as the jurisdiction.
- Choose substance involvement filters for heroin (T40.1), natural and semisynthetic opioids (T40.2), and methadone (T40.3).
- Extract the 2025 annual counts for each category.
- Sum T40.2 and T40.3 to form the prescription opioids group.
- Compare the summed prescription opioid count to the heroin count.
Cross reference with Georgia OASIS definitions to confirm that T40.1 is heroin, T40.2 is natural and semisynthetic opioids, and T40.3 is methadone, ensuring alignment with how Georgia conceptualizes these categories.
The Bigger Picture: A Fentanyl Dominant Era
While prescription opioids exceed heroin in a head to head comparison, both are secondary to fentanyl in Georgia’s 2025 overdose landscape.
Fentanyl’s spread across the illicit drug market, including contamination of stimulants like cocaine and methamphetamine, has accelerated overdose deaths since 2020.
The Georgia Department of Public Health documents this shift explicitly, noting that the post 2020 acceleration reflects fentanyl’s ubiquity rather than a single drug class problem.
This context matters because effective policy cannot frame 2025 as “heroin versus prescription opioids.”
Instead, Georgia needs a comprehensive strategy that positions fentanyl as the dominant threat while incorporating customized interventions for prescription opioid risks (especially in older and rural populations) and persistent heroin related harms (in some urban and vulnerable settings).
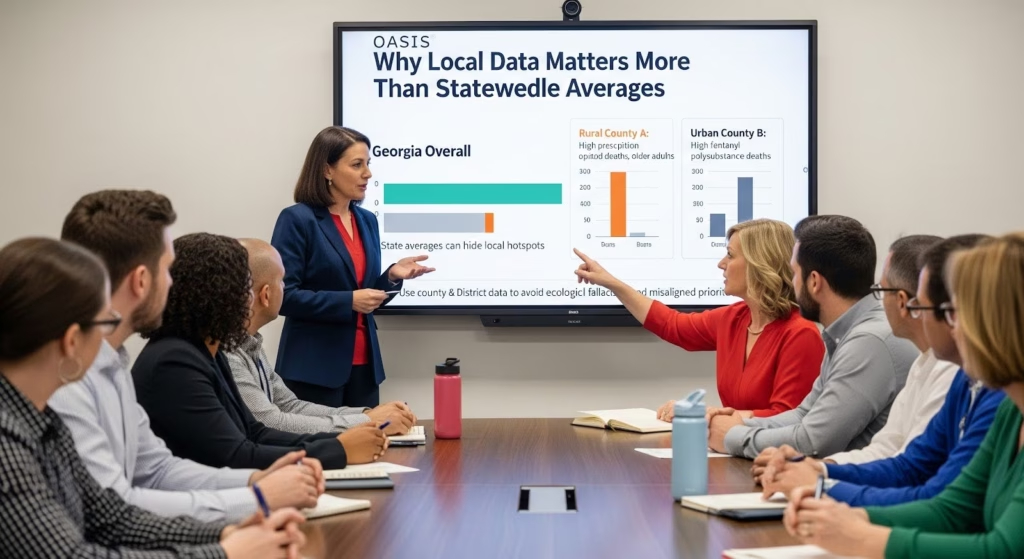
County and District Variation: Why Local Data Matters?
Statewide averages can obscure critical local patterns. Rural counties may show higher per capita rates for prescription opioid deaths among older adults, while urban counties exhibit higher counts and stronger fentanyl driven polysubstance patterns.
The OASIS mapping tool provides residence based county and district views, allowing local health departments to tailor prevention and treatment to their communities.
Sub state analysis is essential to avoid ecological fallacies, where statewide conclusions are applied inappropriately to local contexts.
For example, a county with a high heroin burden should not deprioritize harm reduction services simply because the statewide prescription opioid count is higher.
Limitations and Future Directions
This analysis has several limitations:
- Precision versus directionality: This report provides a methodological and directional conclusion (prescription opioids exceed heroin) without reproducing exact numeric counts, which are retrievable from SUDORS final 2025 data for Georgia.
- Sub state variation: County and public health district patterns may deviate from statewide proportions, requiring local data for operational planning.
- Continuous improvement: As toxicology capabilities advance and coding guidance evolves, comparability over time may be affected. Analysts should consult the SUDORS dashboard’s data considerations for each analytic period.
Future work should integrate SUDORS toxicology detail with Georgia OASIS county level mapping to identify emerging patterns, such as xylazine co involvement or shifts in the heroin versus prescription balance at sub state levels.
Why Does This Comparison Matter for Georgia Families and Communities?
Understanding which opioids drive mortality helps families recognize risk, clinicians adjust prescribing, and policymakers allocate resources.
For a parent whose adult child takes prescription pain medication, knowing that prescription opioids involve more deaths than heroin in Georgia underscores the importance of safe storage, naloxone access, and open conversations about overdose risk.
For a clinician managing chronic pain, it reinforces the value of PDMP checks, non opioid alternatives, and careful tapering.
For people who use heroin, the finding does not diminish their risk. Heroin remains dangerous, especially with fentanyl contamination, and harm reduction services, syringe programs, and MOUD access are lifesaving.
The comparison simply clarifies where the larger burden lies in 2025, guiding prevention priorities without abandoning any population.
Moving Forward: Integrated Strategies for Georgia’s Opioid Crisis
Georgia’s 2025 opioid mortality picture demands integrated action:
- Strengthen prescription opioid stewardship through PDMP utilization, prescriber education, and patient centered pain management.
- Expand MOUD access by co-locating buprenorphine, methadone, and naltrexone with primary care and behavioral health.
- Distribute naloxone universally to patients on high dose opioids, people who use drugs, and their families.
- Advance harm reduction with fentanyl test strips, syringe services, and overdose education personalized to local drug markets.
- Address equity by using SUDORS demographic detail and OASIS sub state resources to target high burden populations with culturally responsive interventions.
- Monitor continuously by triangulating SUDORS, OASIS, and Georgia DPH publications to detect shifts in the heroin versus prescription balance and emerging threats like xylazine.
These strategies recognize that while prescription opioids exceed heroin in 2025 Georgia, both are embedded in a fentanyl dominant, polysubstance landscape that requires comprehensive, evidence based responses.
If you or someone you care about is struggling with opioid use, help is available. Thoroughbred Wellness & Recovery in Marietta offers dual diagnosis treatment that addresses both substance use and mental health, with medical detox, outpatient programs, and holistic therapies tailored to your needs. Call 678-967-0348 anytime, day or night, to start your journey toward freedom.