If you live with bipolar disorder and use cocaine, you may have noticed that your mood swings feel more intense, your medications seem less effective, and your episodes happen more often.
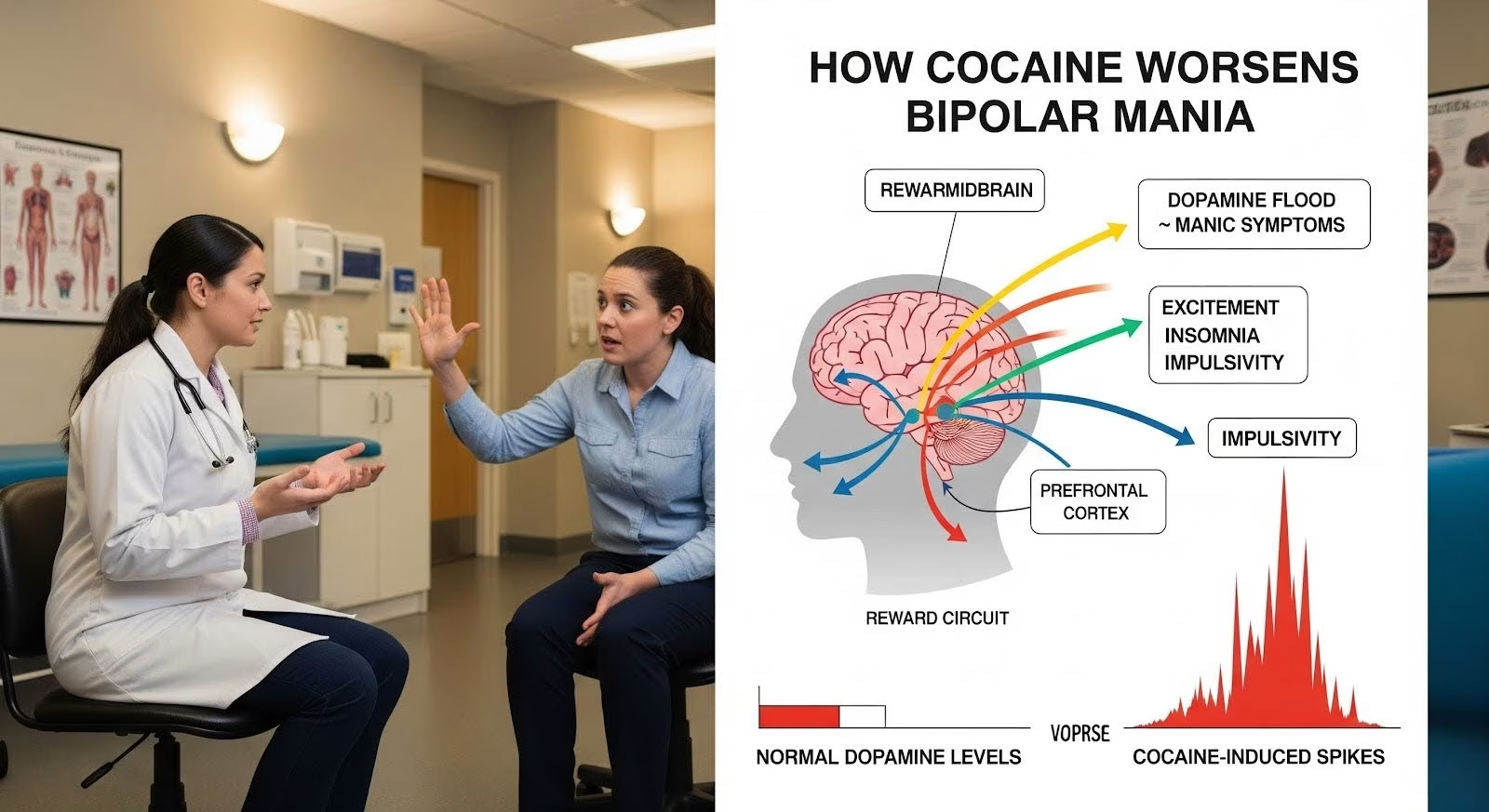
Cocaine amplifies dopamine signaling in the brain’s reward circuits, closely mimicking and worsening manic symptoms like excitement, insomnia, and impulsivity, while early abstinence triggers objective sleep deterioration that can precipitate new mood episodes.
This article explains the neurobiological pathways linking cocaine to bipolar destabilization, reviews evidence on medication and behavioral treatments, and outlines practical strategies to stabilize mood and reduce relapse risk.
Why is Cocaine Especially Dangerous for People With Bipolar Disorder?
Bipolar disorder increases your risk of illicit drug use approximately fivefold compared to the general population, with cocaine being one of the most commonly used substances.
This relationship runs both ways: having bipolar disorder makes you more vulnerable to cocaine use, and using cocaine makes your bipolar symptoms significantly worse.
Research shows that people with bipolar disorder who use cocaine experience more hospitalizations, poorer response to lithium, and greater overall illness burden than those without substance use.
In one study, cocaine users with comorbid bipolar disorder had more lifetime months of cocaine abuse and greater drug use during treatment compared to cocaine users without bipolar disorder.
The clinical burden extends beyond mood symptoms. Substance use in severe mental illness correlates with medication nonadherence, unstable housing, legal problems, and elevated suicide risk.
These social and behavioral consequences further undermine treatment stability, creating a cycle that is difficult to break without integrated care.
How Cocaine Triggers and Worsens Manic Episodes?
Cocaine’s effects on dopamine systems can closely mimic and intensify manic symptoms in people with bipolar disorder. Understanding how stimulant use disrupts brain reward pathways and destabilizes mood regulation is essential for recognizing and managing co-occurring substance use and mania:
Dopamine Amplification and Manic Symptoms
Cocaine intoxication can closely mimic acute mania, producing excitement, grandiosity, emotional lability, delusions, and insomnia.
Both conditions share underpinnings in dopaminergic hyperactivity in brain reward and psychosis circuits.
When you use cocaine, it blocks dopamine transporters, flooding your synapses with dopamine. Chronic cocaine use upregulates dopamine transporter function as your brain tries to compensate for this overflow.
When this homeostatic control fails during extreme stress or high-dose exposure, it can precipitate functional hyperdopaminergia and excited delirium, states with marked agitation and autonomic instability that parallel severe manic episodes.
PET studies in medicated manic patients show abnormal activation in the dorsal anterior cingulate cortex, frontal polar regions, and right inferior frontal areas.
Task-related ACC activation correlates with mania severity, potentially reflecting heightened nucleus accumbens dopamine signaling.
Genetic linkage near the dopamine transporter locus and reports of lower transporter expression in bipolar disorder further support the role of dopamine dysregulation in bipolar pathophysiology.
Postsynaptic Sensitization in Bipolar Disorder
Historic and translational observations indicate that dopamine agonism can induce hypomania or mania in people with bipolar disorder.
L-dopa-induced hypomania and amphetamine-induced arousal have been documented, while catecholamine depletion interacts with lithium’s antimanic effects.
This suggests postsynaptic dopaminergic sensitization in bipolar disorder, rendering you particularly vulnerable to stimulant-triggered mood switches.
Cocaine, as a potent dopamine reuptake inhibitor, can more readily precipitate mania or mixed states in people with bipolar disorder than in those without the condition, especially under conditions of sleep disruption or stress that further bias dopaminergic signaling.
The Sleep and Circadian Connection
Sleep disturbances and disruptions to the body’s natural rhythms are deeply intertwined with both cocaine abstinence and manic episodes. Understanding how these factors influence mood stability and relapse risk is crucial for developing effective interventions that support sustained recovery:
Early Abstinence Insomnia: A Hidden Danger
One of the most critical yet overlooked risks occurs when you stop using cocaine. Multi-study analyses show that between week one and week three of abstinence, chronic cocaine users experience significantly worse objective sleep: decreased total sleep time and sleep efficiency, increased sleep-onset latency, and increased REM latency.
The paradox is that subjective ratings of sleep quality improve during this same period, masking the risk. This “occult insomnia” means you may feel like you’re sleeping better while polysomnography shows your sleep is actually deteriorating.
This first two to three weeks of cocaine abstinence constitutes a high-risk window for mood destabilization, impaired cognition, and relapse.
In a larger polysomnographic characterization of cocaine users in treatment, similar early abstinence sleep deterioration was observed, with modeling suggesting potential recovery in total sleep time only with extended abstinence beyond six weeks.
These findings reinforce the importance of early abstinence sleep-focused interventions as essential to preventing relapse.
Sleep Deprivation as a Manic Trigger
Sleep disruption is a hallmark of mania, and sleep deprivation can precipitate manic switches in bipolar disorder. Circadian phase shifts have been documented in mania and mixed states and normalize with treatment.
In a randomized controlled trial, blue-blocking glasses reduced manic symptoms, highlighting circadian entrainment as an antimanic strategy.
Clock and circadian systems modulate dopaminergic tone. In animal models, CLOCK gene perturbations produce mania-like behaviors and alter ventral tegmental area dopamine neuronal firing. Daytime dopaminergic spikes can drive rapid mood cycling in mice.
Sleep deprivation, a canonical circadian stressor, can trigger mania in bipolar disorder, underscoring the bidirectional link between circadian disruption and dopaminergic behavioral sensitization.

Cross-Sensitization: How Stress, Mood Episodes, and Cocaine Amplify Each Other
Cross-sensitization posits that sensitization acquired in one domain increases responsiveness in another.
Convergent preclinical and clinical data support cross-sensitization among intermittent stressors, mood episodes, and psychostimulant use, leading to mutually reinforcing cycles of increased reactivity, relapse propensity, and illness progression.
This triad of cross-sensitization mechanisms is especially relevant for bipolar disorder with cocaine use disorder.
Stress often triggers cocaine craving and use, cocaine destabilizes mood circuits, and mood episodes sensitize stress and reward pathways. Together, these processes amplify relapse risk across both disorders.
The allostatic load framework captures the cumulative cost of chronic adaptation to stress, episodes, and substance exposure.
Repeated perturbations require systemic recalibration of the HPA axis, neurotransmitter systems, and immune signaling, which progressively taxes neural circuits supporting mood regulation, cognition, and reward. This heightens vulnerability to further episodes and substance use.
Stress-induced activation of the HPA axis predicts cocaine craving and relapse. In women with crack cocaine addiction, polymorphisms in glucocorticoid receptor system genes modulated depressive symptom severity during early abstinence and influenced rehospitalization rates, implicating stress-genetic susceptibility in mood destabilization during cocaine withdrawal.
Distinguishing Cocaine Intoxication From Primary Mania
Cocaine intoxication can closely resemble acute mania, complicating diagnosis and treatment planning. Understanding the differences is critical for appropriate care.
Time course and trigger: Manic episodes typically last days to weeks, while cocaine intoxication peaks within hours, with residual stimulant effects lasting up to one to two days depending on dose and route.
Substance-induced mania should temporally align with intoxication or withdrawal. Persistent syndromal mania beyond pharmacological windows suggests primary bipolar disorder.
Sleep signature: Acute cocaine use induces sleep loss followed by an abnormal early abstinence course with worsened objective sleep.
Mania is classically associated with reduced need for sleep and shortening of REM latency during switches. In early abstinence, polysomnographic REM latency increases, differentiating it from typical manic REM changes and emphasizing the need for objective sleep assessments.
Psychosis content and autonomic instability: Severe autonomic dysregulation, hyperthermia, and delirium point to stimulant toxicity or excited delirium rather than primary mania.
Such cases require medical stabilization, not psychiatric activation or exercise. Rhabdomyolysis risk in excited delirium and severe mania further supports cautious, medical-first management in unstable presentations.
| Feature | Cocaine Intoxication | Early Cocaine Withdrawal | Primary Mania |
| Onset/Duration | Minutes to hours post-use; brief to 1–2 days | Days to weeks post-cessation | Days to weeks (episodes) |
| Arousal/Sleep | Marked insomnia, agitation | Objective sleep worsens despite subjective improvement | Reduced need for sleep; shortened REM latency |
| Psychosis | Paranoia, hallucinations common; delirium possible | Dysphoria; vivid dreams; less often florid psychosis | Psychosis possible in severe mania |
| Autonomic signs | Tachycardia, hyperthermia, instability; arrhythmia risk | Normalizing autonomics; fatigue/dysphoria | Usually less severe autonomic instability |
| Temporal link | Aligned with recent use | Aligned with cessation window, weeks 1–3 | Not contingent on recent substance timing |
Medication Strategies: What Works and What Doesn’t
Finding effective medication strategies for co-occurring bipolar disorder and cocaine dependence is complex, with some treatments showing modest benefits while others require further research. Understanding the nuances of lamotrigine and other pharmacotherapies is crucial for guiding clinical decisions and managing patient expectations:
Lamotrigine: Modest Effects on Cocaine Use
The most robust randomized controlled trial in bipolar disorder with comorbid cocaine dependence randomized 120 outpatients in depressed or mixed states to lamotrigine (up to 400 mg/day) or placebo for 10 weeks.
The primary outcome, urine drug screens, and mood ratings did not differ significantly between groups. However, self-reported dollars spent on cocaine decreased more with lamotrigine both initially and across weeks one to ten.
Earlier open-label studies found lamotrigine associated with improvement in depressive and manic symptoms and cocaine craving, with mixed findings on actual use.
The RCT suggests lamotrigine, a standard mood stabilizer for bipolar depression, might reduce the amount spent on cocaine without significantly altering verified abstinence or mood at 10 weeks.
Clinical takeaway: Lamotrigine may indirectly reduce cocaine spending, perhaps via mood stabilization and craving reduction, but does not reliably increase cocaine-negative urines or improve mood symptoms versus placebo over 10 weeks.
It remains a reasonable choice for bipolar depression in this population, but its anticocaine effect is limited and insufficient as a sole strategy.
Other Pharmacotherapies
Citicoline: In randomized trials involving bipolar disorder with cocaine dependence, citicoline reduced cocaine-positive urines or active use and the likelihood of relapse, without significant effects on mood or craving measures. Although promising for cocaine metrics, replication and broader availability remain concerns.
Valproate: Pilot work suggested utility in bipolar disorder with co-occurring cocaine dependence, but the evidence base is limited and not specific to cocaine outcomes. Valproate remains valuable for mood stabilization and may indirectly reduce use by stabilizing mood.
Atypical antipsychotics: Quetiapine and risperidone have been associated with improvements in mood symptoms and craving in bipolar disorder with stimulant use, but randomized, placebo-controlled evidence for cocaine outcomes is sparse. Mood symptom control remains their primary role.
A 2019 systematic review of pharmacotherapies for co-occurring substance use disorder and bipolar disorder concluded that valproate sodium and lamotrigine may be preferred agents for combined psychiatric and substance outcomes, but most available studies are open-label with modest sample sizes.
The review emphasized the preliminary nature of recommendations and the need for larger, well-controlled trials.
Behavioral Treatments That Actually Work
Effective behavioral treatments for substance use disorders, particularly for those with co-occurring mental health conditions, focus on tangible incentives and integrated therapeutic approaches. Contingency management and specialized group therapies offer proven strategies to increase abstinence, improve retention, and reduce relapse risk:
Contingency Management: The Gold Standard
Contingency management provides tangible incentives (vouchers or prizes) contingent on verified abstinence (negative urine samples) or attendance.
Meta-analyses and randomized controlled trials demonstrate that CM increases abstinence rates, extends longest duration of abstinence, and improves retention.
In cocaine-dependent samples, high-magnitude abstinence-based reinforcement yields the most robust effects for patients who begin treatment while using.
For those entering abstinent, both attendance-based and abstinence-based CM can improve outcomes on some measures. Notably, longest duration of abstinence during CM predicts abstinence at follow-up, validating it as a clinically meaningful target.
CM also generalizes to dual-diagnosis populations. In a randomized study of cocaine-dependent patients with severe and persistent mental health disorders, including bipolar disorder, CM produced significantly more continuous weeks abstinent (mean 2.9 versus 0.6) than testing-only controls and higher proportions of cocaine-negative samples.
Larger implementation efforts in Veterans Administration systems show feasibility and dissemination potential.
Integrated Group Therapy for Bipolar Disorder and Substance Use
Integrated Group Therapy is a manualized, cognitive-behaviorally informed group therapy tailored for bipolar disorder with substance use disorder that targets both disorders simultaneously. It reframes them as a single “bipolar substance abuse” condition with shared relapse processes.
Across three trials, including two randomized controlled trials and a “community-friendly” version, IGT outperformed control conditions (such as group drug counseling) on substance and mood outcomes and improved retention.
IGT emphasizes medication adherence, symptom recognition, relapse prevention skills, and the explicit interdependence of bipolar disorder and substance use disorder. Its structure and brevity (12 sessions) support translation to routine care.
Practical Steps to Stabilize Mood and Reduce Relapse
Stabilizing mood and preventing relapse in individuals with co-occurring bipolar disorder and stimulant use requires a multi-faceted approach. This includes early mood stabilization, aggressive management of sleep and circadian rhythms, high-magnitude contingency management, integrated psychotherapy, and digital monitoring to identify early warning signs:
Early and Sustained Mood Stabilization
Optimize mood stabilization promptly based on your current phase. Consider lamotrigine for bipolar depression and valproate for mixed or rapid cycling states, recognizing limited direct effects on cocaine use but critical benefits for mood stability. Lithium remains valuable for mania maintenance and has suicide prevention benefits.
Aggressive Sleep and Circadian Stabilization
Given abstinence-related insomnia and mania risk, prioritize sleep-protective strategies:
- Psychoeducation on sleep hygiene and structured sleep-wake routines
- Light management, such as blue-blocking glasses in evenings
- Cautious use of sedating antipsychotics (for example, quetiapine in bipolar depression with insomnia) as clinically appropriate
- Avoid benzodiazepine escalation and sedative misuse
- Consider objective sleep monitoring with wearables or actigraphy during early abstinence
High-Magnitude Contingency Management
Start high-magnitude, abstinence-based CM (at least $500 equivalent over 12 weeks) with twice-weekly urine drug screens.
If your baseline urine drug screen is negative, combine attendance-based and abstinence-based CM. Measure and aim to extend your longest duration of abstinence, as this predicts long-term success.
Integrated Psychotherapy
Enroll in Integrated Group Therapy to consolidate skills bridging bipolar disorder and substance use disorder. Emphasize medication adherence, trigger management, and sleep and circadian regularity. The 12-session structure makes it practical for routine care settings.
Digital Monitoring and Early Warning Systems
Ecological momentary assessment via smartphones can track within-person variability in mood, sleep, stress, energy, and impulsivity. EMA can capture dynamic transitions, such as rising impulsivity with sleep reduction predicting next-day mood symptoms.
For bipolar disorder with stimulant comorbidity, integrating EMA prompts around craving, stress, and sleep can flag high-risk windows for contingency management reinforcement and clinical outreach.
Address Social Determinants
Coordinate across psychiatry, addiction services, and social supports to address nonadherence, housing, legal issues, and suicidality proactively. Reducing stressors that fuel cross-sensitization improves adherence and outcomes.

Why is Integrated Care Essential?
Guideline bodies and best-practice syntheses recommend integrated care for coexisting severe mental illness and substance use, emphasizing coordinated assessment, confidentiality, crisis planning, and parallel attention to both conditions.
A “no wrong door” system mandates routine screening for substance use disorder in mental health settings and vice versa, ensuring identification, assessment, and linkage to treatment regardless of entry point.
People with co-occurring disorders are more frequently hospitalized. Early detection and integrated treatment are associated with improved outcomes across psychiatric and substance use domains.
Substance use in severe mental illnesses also relates to nonadherence with psychiatric medications, criminal behavior, homelessness, and suicide, compounding the direct effects of stimulants on neural systems.
Based on the totality of high-quality evidence, pharmacotherapy alone, while essential for mood stabilization, does not meaningfully reduce cocaine use in bipolar disorder.
The most impactful and implementable approach today is to combine high-magnitude, abstinence-based contingency management with bipolar disorder-specific Integrated Group Therapy, delivered within an integrated care framework that simultaneously optimizes mood stabilizers and addresses social determinants.
Moving Forward With Confidence
Cocaine use and bipolar disorder create a vicious cycle through dopaminergic amplification, circadian and sleep disruption, and cross-sensitization among stress, mood episodes, and substance use.
Each domain feeds the others, progressively taxing neural circuits and heightening vulnerability to further episodes and relapse.
Breaking this cycle requires early, persistent application of an integrated model: optimize mood stabilizers, implement high-magnitude contingency management, enroll in Integrated Group Therapy, stabilize sleep and circadian rhythms aggressively during early abstinence, and use digital monitoring to detect and respond to early warning signs.
This approach offers the best chance to stabilize mood, prolong abstinence, and mitigate illness progression.
If you or someone you care about is navigating bipolar disorder and cocaine use, know that evidence-based, compassionate care can make a profound difference.
Reach out today to explore Thoroughbred Wellness and Recovery’s dual diagnosis treatment that addresses both conditions simultaneously and supports lasting recovery.