Detox costs can feel overwhelming when you or someone you love needs help right away.
In 2025, the national average for detoxification services is about $525 per day, with seven‑day programs ranging from roughly $3,675 for basic outpatient care to $10,000 or more for hospital‑based or rapid detox.
This guide breaks down what drives those costs, how insurance coverage works, and what you can expect to pay out of pocket.
What Determines the Cost of Detox?
The price you pay for detox depends on several factors that shape the intensity and setting of care. Understanding these drivers helps you anticipate costs and choose the right level of support.
Level of Care and Medical Intensity
Detox programs follow clinical standards that define staffing, monitoring, and medical oversight. The ASAM Criteria organizes withdrawal management into levels based on how much medical supervision you need.
Lower‑intensity outpatient programs cost less because they require fewer nursing hours and less equipment.
Higher‑acuity settings like medically monitored inpatient units or hospital‑based detox involve 24‑hour nursing, physician availability, continuous vital sign monitoring, and sometimes intensive care backup, all of which increase daily rates.
How Much is Detoxing? Setting: Outpatient, Inpatient, or Hospital
Where you receive detox makes a big difference in cost. Outpatient detox lets you stay at home and attend daytime sessions, typically costing $250 to $500 per day.
Inpatient residential detox provides round‑the‑clock support in a facility, with daily rates from $250 to $800 depending on medical staffing.
Hospital or ICU‑based detox is reserved for severe withdrawal complications like seizures or delirium tremens and can run $5,000 to $10,000 for a five‑ to seven‑day stay.
Geographic Location and Labor Costs
Detox prices vary by region. Urban centers and coastal markets often charge more due to higher wages, rent, and demand.
Rural areas may offer lower base prices but fewer nearby options. The Bureau of Labor Statistics publishes regional wage data that illustrate these differences; higher nursing and clinical staff salaries in metro areas translate directly into higher per‑diem rates.
Amenities and Facility Type
Luxury detox centers start around $10,000 and climb with private rooms, spa services, and holistic therapies.
Public or state‑funded programs may provide low‑cost or no‑cost services for eligible individuals, though waitlists can be long. Private facilities offer more flexibility and amenities at higher prices.
Average Detox Costs by Program Type in 2025
The table below summarizes typical costs across common detox settings, drawn from consumer cost syntheses and industry reviews.
| Program Type | Daily Cost | Typical Total (7 days) | Notes |
| Outpatient detox | $250–$500 | $1,000–$1,500 (4–6 days) | Daytime services; patient at home; lower medical risk |
| Standard inpatient detox | $250–$800 | $1,750–$5,600 | 24/7 supportive care; variable medical monitoring |
| Supervised medical detox | $500–$650 | $3,500–$4,550 | 24/7 nursing with physician oversight; higher intensity |
| Hospital/ICU detox | N/A | $5,000–$10,000 (5–7 days) | Medically necessary for severe withdrawal; often covered |
| Rapid detox | N/A | $5,000–$10,000 | Anesthesia-assisted; controversial due to risks |
| Luxury detox | Starts ~$10,000 | Often >$10,000 | Premium amenities and privacy |
These ranges reflect the national average of approximately $525 per day, with substantial variation by clinical complexity and setting.
How Insurance Covers Detox and What You Pay
Insurance coverage can dramatically reduce your out‑of‑pocket costs, but the details matter. Here’s how different coverage types work in 2025.
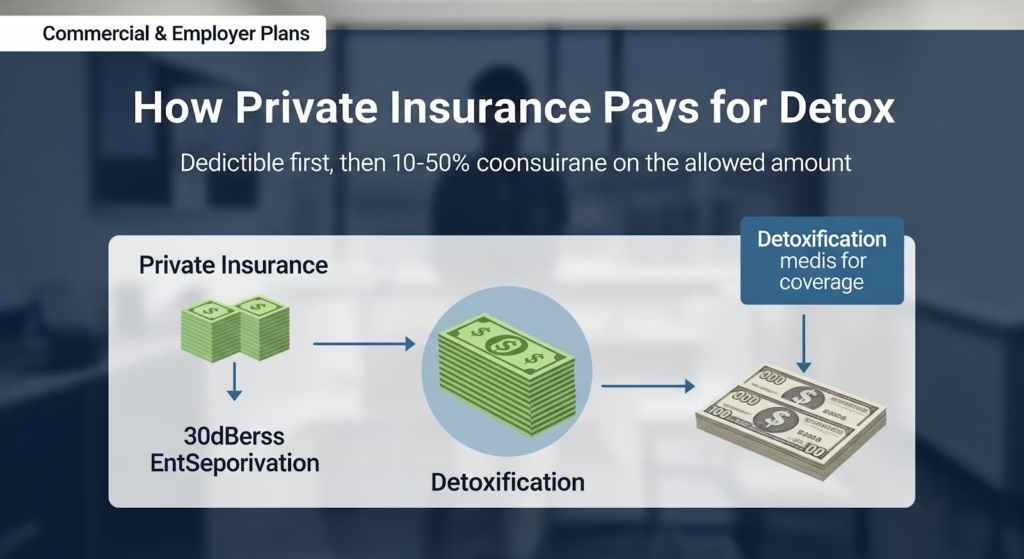
Commercial and Employer Plans
Most commercial health plans cover medically necessary detox as part of mental health and substance use disorder benefits.
The Affordable Care Act requires individual and small‑group plans to include these services as essential health benefits.
The Mental Health Parity and Addiction Equity Act (MHPAEA) ensures that financial requirements like deductibles, copays, and coinsurance for detox cannot be more restrictive than those for medical or surgical care.
In practice, you’ll typically pay a deductible first, then coinsurance (often 10% to 50%) on the allowed amount.
For example, if your plan’s in‑network allowed amount for a seven‑day supervised medical detox is $3,500 and you have a $1,500 deductible with 20% coinsurance, you would pay $1,500 plus 20% of the remaining $2,000, totaling $1,900.
Out‑of‑network care triggers higher cost‑sharing unless emergency protections apply.
Medicaid Coverage
Medicaid generally covers medically necessary detox for eligible members, often with minimal or no cost‑sharing. States negotiate rates with providers, and coverage details vary by state and managed care plan.
For instance, California’s Medi‑Cal Behavioral Health fee schedules show county‑level reimbursement structures for withdrawal management, while Texas Medicaid publishes fee lookup tools that illustrate allowable amounts by service category.
If you’re eligible, Medicaid can cover the full cost of detox, making it one of the most affordable pathways.
Medicare
Medicare Part A covers hospital‑based detox under inpatient prospective payment system (IPPS) rules, with payment determined by diagnosis‑related groups (DRGs) and adjusted for local wage indexes.
Professional services are paid under the Medicare Physician Fee Schedule. Beneficiaries pay deductibles and coinsurance according to their plan design.
No Surprises Act Protections
If you need emergency detox and receive care at an out‑of‑network hospital, the No Surprises Act limits your cost‑sharing to in‑network levels and prohibits balance billing.
This protection is critical for unplanned, urgent withdrawal episodes that require hospital admission.
What You’ll Pay Out of Pocket: Real Scenarios
Understanding how deductibles and coinsurance work helps you estimate your actual costs. Here are four common scenarios based on 2025 plan designs.
Outpatient Detox, In‑Network
Five days at $350 per day allowed amount; plan has a $1,500 deductible and 20% coinsurance. If your deductible is not yet met, the first four days ($1,400) apply to the deductible, and day five triggers 20% coinsurance on $350, or $70. Your total: about $1,470. If the deductible is already met, you pay 20% of $1,750, or $350.
Standard Inpatient Detox, In‑Network
Seven days at $500 per day allowed ($3,500 total); plan has a $2,500 deductible and 20% coinsurance. If the deductible is not met, you pay $2,500 plus 20% of the remaining $1,000, totaling $2,700. If the deductible is met, you pay 20% of $3,500, or $700.
Hospital Detox, Emergency, Out‑of‑Network
Five‑day emergency admission; hospital charges $20,000, but the plan’s in‑network allowed amount benchmark is $10,000. Under the No Surprises Act, you pay in‑network cost‑sharing: a $500 copay plus 20% coinsurance on $9,500, totaling $2,400. You are not billed the $10,000 difference.
Self‑Pay with Good‑Faith Estimate
Rapid detox priced at $7,500; provider issues a good‑faith estimate. Final bill is $8,200, a $700 difference. Because the difference exceeds $400, you can file a patient‑provider dispute resolution request within 120 days for an independent review.
How Mental Health Parity Rules Affect Detox Access and Costs?
The 2024 MHPAEA final rules strengthen protections for substance use disorder care. Plans must ensure that nonquantitative treatment limitations (NQTLs) like prior authorization, network adequacy, and facility‑type restrictions are no more stringent for mental health and SUD benefits than for medical and surgical care.
Plans must also collect and evaluate outcomes data to identify and fix access disparities.
For detox, this means insurers are under pressure to contract with enough in‑network providers, streamline authorization processes, and ensure that out‑of‑network reimbursement methodologies don’t push patients toward high out‑of‑pocket costs.
While many provisions apply by the first plan year on or after January 1, 2026, the statutory parity framework is already in effect.
Expect continued improvements in network breadth and authorization speed over the next year.

Tips to Reduce Your Detox Costs
- Verify network status early. Confirm that the facility and all clinicians (physicians, nurses, anesthesiologists) are in your plan’s network. Review your Summary of Benefits and Coverage for deductibles and coinsurance.
- Ask about medical necessity and level of care. Ensure your clinical presentation aligns with the appropriate ASAM level and that documentation supports the need for the setting you’re entering. This helps with authorization and coverage.
- Use emergency protections when applicable. For severe withdrawal requiring urgent hospital care, emergency services are protected against balance billing under the No Surprises Act.
- Request a good‑faith estimate if paying out of pocket. Keep documentation; if your final bill exceeds the estimate by $400 or more, you can dispute it within 120 days.
- Explore public programs. Check Medicaid eligibility, county behavioral health networks, or state‑funded slots that may cover most or all costs.
- Contact SAMHSA for guidance. The Substance Abuse and Mental Health Services Administration offers FindTreatment.gov and the 988 crisis line to help you find appropriate care quickly.
Looking Ahead: Parity and Access in 2025–2026
In my assessment, the most important trend shaping detox costs in 2025 is not a change in provider base rates but the expansion of in‑network access driven by parity enforcement.
The 2024 MHPAEA final rules require plans to demonstrate adequate network composition and to remediate access barriers when outcomes data show disparities.
This should increase the number of in‑network detox providers, particularly for higher‑acuity medically monitored and hospital‑based withdrawal management, and reduce the likelihood that patients face out‑of‑network cost‑sharing or balance billing.
Base provider charges will continue to reflect clinical complexity, staffing intensity, and regional labor costs. Higher‑acuity programs will remain more expensive because they require more resources.
But for patients, the variable that matters most is whether care is in‑network and whether authorization is timely. Parity improvements should stabilize and, in many cases, reduce out‑of‑pocket liabilities by making in‑network detox more accessible and predictable.
Take the Next Step Toward Recovery
Detox is the critical first step, but lasting recovery requires ongoing support. If you or someone you care about is ready to begin treatment, reach out to a detox program that offers a full continuum of care, from medical detox through outpatient services, with compassionate, personalized support. Contact our team to verify your insurance, discuss your options, and start your journey toward freedom today.