Many people seeking behavioral health treatment wonder what an Intensive Outpatient Program actually requires.
An IOP typically demands at least nine hours of structured therapy per week, often delivered as three three-hour sessions, while allowing you to live at home and maintain work or family responsibilities.
This article explains the core requirements, how they differ across providers and payers, and what you can do to meet them successfully.
What is an Intensive Outpatient Program?
An Intensive Outpatient Program is a structured, non-residential behavioral health regimen that sits between standard weekly therapy and full-time residential care.
IOPs are classified as Level 2.1 care under the American Society of Addiction Medicine (ASAM) criteria and deliver multimodal services including group therapy, individual counseling, psychoeducation, family engagement, case management, and medication-assisted treatment when appropriate.
For adults, the minimum weekly dose is commonly set at nine hours, typically delivered as three sessions of about three hours each.
Programs follow ASAM’s six-dimensional assessment, covering intoxication/withdrawal potential, biomedical conditions, emotional/behavioral/cognitive conditions, readiness to change, relapse/continued use potential, and recovery environment, to determine whether IOP is the right level of care for you.
Core IOP Requirements You Should Expect
Understanding what high‑quality opioid treatment programs must provide helps patients and families advocate for safe, evidence‑based care. Clear expectations around counseling, medication management, and monitoring protect against substandard or unsafe practices:
Weekly Time Commitment and Scheduling
Most adult IOPs require at least nine hours of services per week, often arranged as three three-hour sessions. This intensity distinguishes IOP from routine outpatient therapy but remains below the 20-plus hours per week required for partial hospitalization programs.
For employed, caregiving, or school-enrolled patients, daytime schedules can conflict with work, childcare, and transportation windows, creating one of the most common barriers to consistent attendance.
Evening telehealth IOPs, typically three to five evenings per week, with approximately three hours per session, have emerged to reduce scheduling conflict and may improve attendance for those with daytime constraints. Hybrid delivery further allows you to attend in person as needed and to leverage telehealth for convenience and continuity.
Clinical Content and Services
SAMHSA guidance indicates that IOP outcomes can be comparable to residential care for appropriately selected clients.
Programs emphasize features that improve engagement and retention: case management, family psychoeducation, peer services, linkage to medication-assisted treatment, and trauma-focused care.
Typical program elements include process groups, psychoeducation, skills training, family support, medication management, and case management, all of which influence attendance and retention.
Documentation and Medical Necessity
Medicare’s outpatient psychiatric coverage standards apply to IOP and require an individualized, physician-prescribed plan of treatment specifying type, amount, frequency, and duration, with periodic physician evaluation and supervision of therapists and staff.
Coverage requires a reasonable expectation of improvement or prevention of relapse/hospitalization per documented clinical progress. Non-covered services include meals, transportation, purely recreational activities, and psychosocial/vocational programs.
How IOP Requirements Differ by Provider Type
Hospitals, community mental health centers, and private OTPs all operate under the same federal framework but apply requirements differently. Knowing how expectations vary by setting helps patients choose programs that match their needs and circumstances:
Hospitals and Critical Access Hospitals
Hospitals bill IOP using institutional claims with Condition Code 92 and revenue code 0905, reporting HCPCS codes for covered services at the line level.
Payment is made via Outpatient Prospective Payment System APCs stratified by the daily number of distinct IOP services: up to three services per day or four or more services per day.
Critical Access Hospitals follow similar clinical and coverage rules but are paid at 101 percent of reasonable cost and are exempt from line-level HCPCS reporting.
Community Mental Health Centers
Community Mental Health Centers bill with Condition Code 92 and revenue code 0905, using OPPS-aligned per diem payment via APCs similar to hospitals.
CMHCs operate under updated Conditions of Participation that include personnel qualifications changes for mental health counselors and marriage and family therapists, enabling broader staffing participation in IOP.
Federally Qualified Health Centers and Rural Health Clinics
As of January 1, 2024, Medicare covers IOP with payment at the same rate as hospitals for FQHCs and RHCs, with IOP costs excluded from all-inclusive rate and prospective payment system calculations.
These settings must use revenue code 0905 and follow programmatic conditions including scope of benefits, plan-of-care certification, and coding/billing rules.
Payer Variation: Medicare, Medicare Advantage, and Commercial Plans
Coverage for OTP services looks different depending on whether patients have Medicaid, Medicare Advantage, or commercial insurance. These payer variations affect out‑of‑pocket costs, network access, and which supportive services are realistically available:
Medicare’s Standardized IOP Benefit
The Consolidated Appropriations Act of 2023 established Medicare coverage and payment for intensive outpatient program services, implemented through the CY 2024 OPPS/ASC final rule.
This created a per diem IOP benefit for services furnished in hospital outpatient departments, CAH outpatient departments, and CMHCs beginning January 1, 2024, with concurrent policies allowing IOP payment at hospital-equivalent rates for FQHCs and RHCs.
Commercial and Medicare Advantage Differences
Commercial payers often use different revenue and HCPCS code sets than Medicare. For example, some plans list Dual Diagnosis IOP with revenue codes 905 and 906 and identify preferred HCPCS codes S9480 for psychiatric IOP per diem and H0015 for substance use disorder IOP per day, with alternates H0004 and H2036.
Prior authorization depends on the member’s benefit plan, and providers must verify eligibility and benefits and confirm that contracted fee schedules include the applicable revenue and HCPCS/CPT codes.

State-Level Overlays: California and Texas Examples
California and Texas offer contrasting models for regulating mental health and substance use treatment, particularly in areas like telehealth and licensure. Examining these state-level approaches can provide valuable insights for Georgia as it seeks to optimize its own policies and delivery systems:
California’s Telehealth and County Flexibility
California’s Drug Medi-Cal Organized Delivery System agreements establish overall governance, but county contracts do not set granular clinical standards like IOP group size or hours.
The California Department of Health Care Services Behavioral Health Information Notice index is the authoritative repository for updated guidance relevant to DMC-ODS policies, including telehealth and documentation standards.
Under California policy, telehealth is explicitly treated as a delivery mechanism, not a distinct service, to furnish specialty mental health services and SUD treatment. Synchronous and asynchronous modalities are permitted, supporting broad flexibility to deliver covered services as clinically appropriate.
Texas Licensure and Rule Review
Texas regulates chemical dependency treatment facilities under Health & Safety Code Chapter 464, defining chemical dependency, program exemptions, prohibited medical services for exempt programs, and granting the Department of State Health Services authority for inspections and fees.
Providers must meet licensure and inspection requirements, and rule updates for Texas Administrative Code Chapter 448 would appear in the Texas Register with a 31-day public comment window after publication.
The Biggest Challenges Patients Face in Meeting IOP Requirements
Many people receiving methadone or buprenorphine struggle with rigid scheduling, transportation barriers, and complex take‑home rules. These challenges can make it hard to stay in compliance even when patients are motivated to continue treatment:
Time and Scheduling Burdens
The requirement of at least nine hours per week, often arranged as three three-hour sessions, creates opportunity costs such as lost wages and can strain logistics including commuting and recovery housing curfews.
Evening telehealth IOPs are intentionally designed to reduce scheduling conflict and may improve attendance for those with daytime constraints.
Digital Access and Privacy Barriers
When IOPs rely on telehealth, early dropout risk increases among subgroups facing digital barriers. In a large multi-site study during 2020–2021, patients who discontinued within 14 days were more likely male, younger, and with lower education.
Challenges include unreliable broadband or devices, limited digital literacy, and lack of private spaces for group therapy or sensitive disclosures.
High Symptom Burden in Dual Diagnosis
Co-occurring mental health disorders increase dropout vulnerability, especially in the first month of outpatient care.
A 2024 real-world study found 23 to 50 percent dropout in general outpatient SUD care and even higher in dual diagnosis, with approximately 60 percent dropout in the first month and approximately 80 percent in the first year.
Symptoms such as severe anxiety, PTSD-related avoidance, depression, impulsivity, and cognitive load can degrade session attendance, homework completion, and crisis management.
Coverage and Network Adequacy Friction
Even with Medicare’s new IOP benefit, patients experience access friction when local networks are thin, particularly for Medicare Advantage plans and rural areas, when provider billing systems are still adapting, or when utilization management policies create delays.
Fragmented coverage across Medicare, Medicaid, and commercial payers can generate uncertainty over benefits, cost-sharing, and authorized service mix, discouraging consistent attendance and prolonging gaps in care.
Early Engagement Vulnerability
Across outpatient SUD care, early dropout is common, and in dual-diagnosis patients it is particularly high in the first month.
This early attrition window is where attendance requirements are most fragile and where targeted engagement strategies, rapid follow-up, digital readiness support, crisis planning, have a disproportionate impact on completion.
Evidence-Based Solutions That Improve IOP Adherence
Hybrid care models, streamlined dosing protocols, and proactive case management can make it easier for patients to meet OTP rules. These solutions reduce drop‑out risk and support long‑term stabilization on methadone or buprenorphine:
Hybrid Delivery Models
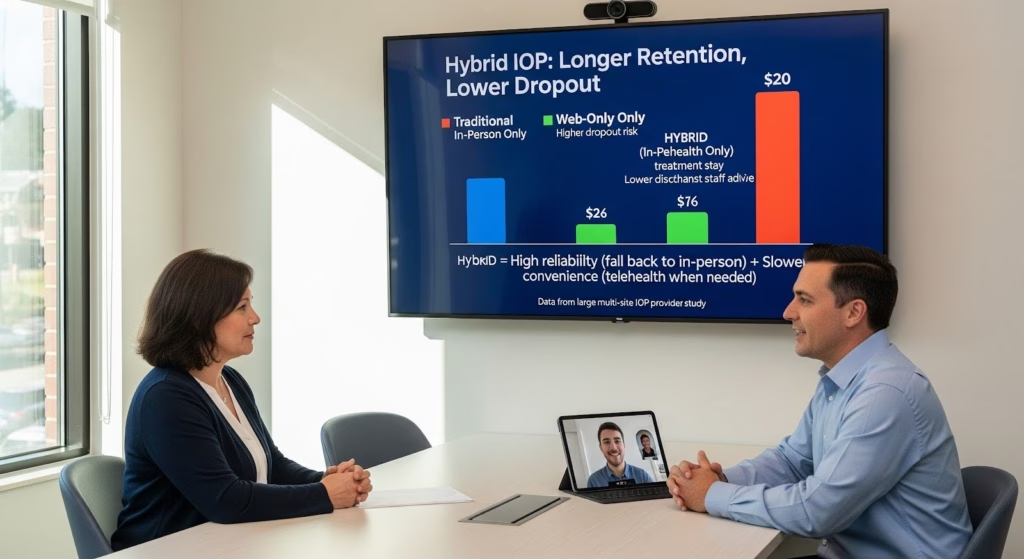
Ecologically valid data from a large multi-site IOP provider found that participants in hybrid IOP stayed in treatment significantly longer and were discharged against staff advice at lower rates than those in traditional in-person or web-only programming.
Hybrid offers high reliability by allowing a fall back to in person when tech or privacy fails and high convenience through telehealth when circumstances block travel.
Integrated Dual-Diagnosis Protocols
An integrated, CBT-based, two-week IOP for veterans with co-occurring SUD and PTSD/mood/anxiety disorders demonstrated substantial symptom reductions and 91 percent retention, with similar benefits across in-person, hybrid, and telehealth delivery.
These data suggest that short, massed, integrated protocols can markedly improve engagement for dual-diagnosis populations traditionally prone to dropout in weekly outpatient formats.
Case Management and Family Engagement
SAMHSA guidance underscored that engagement and retention improve when programs include structured case management, family psychoeducation, peer services, trauma-focused care, and linkage to medication-assisted treatment.
Case management addresses social determinants such as housing instability, transportation, and employment/legal issues that conflict with attendance, while family psychoeducation improves home environment, increases accountability, and reduces conflict that can disrupt participation.
What You Can Do to Meet IOP Requirements Successfully?
Verify your coverage and benefits early. Contact your insurance plan to confirm IOP coverage, cost-sharing, and any prior authorization requirements. For Medicare Advantage plans, ask whether the program is in network and whether telehealth participation is covered.
Ask about evening and hybrid options. If daytime sessions conflict with work or caregiving, inquire whether the program offers evening telehealth IOP or hybrid delivery that allows you to attend in person when needed and via telehealth for convenience.
Request digital inclusion support. If you lack reliable broadband, a private space, or digital literacy, ask the program about device lending, data plan support, pre-session tech checks, and on-site spaces for private virtual participation.
Engage case management from day one. Early case management can address housing, transportation, legal/employment needs, coverage verification, and urine drug screen logistics, reducing external barriers to attendance.
Communicate early if you miss a session. Programs that use routine outcome monitoring and attendance data can trigger intensified support during the high-risk first month. Same-day contact and problem-solving can prevent early dropout.
IOP Requirements at a Glance
| Requirement | Typical expectation | Flexibility options |
| Weekly hours | At least 9 hours, often 3 sessions of 3 hours | Evening schedules; flexible make-up sessions |
| Clinical services | Group therapy, individual counseling, psychoeducation, family support, case management | Hybrid modalities; trauma-focused modules; peer support |
| Documentation | Physician-prescribed plan; periodic evaluation; progress toward goals | Measurement-based care; early intervention for dropout risk |
| Modality | In-person, telehealth, or hybrid | Synchronous/asynchronous telehealth; on-site privacy booths |
| Authorization | Depends on payer; Medicare standardized; commercial plan-specific | Early eligibility verification; pre-service coordination |
Why These Requirements Matter for Your Recovery?
IOP requirements are designed to deliver a dose of care sufficient to stabilize symptoms, reduce relapse risk, and sustain recovery while you remain in your community.
The nine-hour minimum, physician supervision, and individualized treatment planning are not arbitrary, they reflect evidence that this intensity can achieve outcomes comparable to residential care for appropriately selected patients.
When programs pair flexible scheduling with integrated dual-diagnosis protocols, proactive digital inclusion support, and payer-aligned care coordination, they reconcile clinical and regulatory requirements with the lived realities of IOP participants.
This integrated approach targets early dropout risk and dual-diagnosis complexity with precision, translating the established efficacy of IOP into higher completion rates and better long-term outcomes.
If you or a loved one is considering IOP, understanding these requirements and the supports available to meet them can make the difference between early dropout and sustained recovery.
The highest-yield strategy is a hybrid, measurement-driven IOP that pairs flexible scheduling, including evening telehealth, with integrated co-occurring care, proactive digital inclusion support, and structured linkage to medication-assisted treatment.
Ready to explore IOP options that fit your life? Contact Thoroughbred Wellness & Recovery at 678-325-6820 to discuss evening IOP, hybrid delivery, and personalized support designed to help you meet program requirements and achieve lasting freedom.