Methamphetamine withdrawal can feel overwhelming, but understanding what to expect makes the process less frightening.
The acute detox period typically lasts about one week, with peak symptoms appearing within the first 2 to 7 days after last use.
While methamphetamine withdrawal is rarely life threatening on its own, the intense mood changes, sleep disruption, and craving can drive relapse or create indirect risks like suicidality and cardiovascular complications.
This article walks you through the withdrawal timeline, common symptoms, and evidence based strategies to support safe recovery.
What is Meth Withdrawal?
Methamphetamine withdrawal is the body’s response when someone who has been using meth regularly stops or sharply reduces their intake.
The syndrome is highly prevalent among people with methamphetamine dependence, with research showing that roughly 88% of those with dependence report six or more withdrawal signs when the drug becomes unavailable.
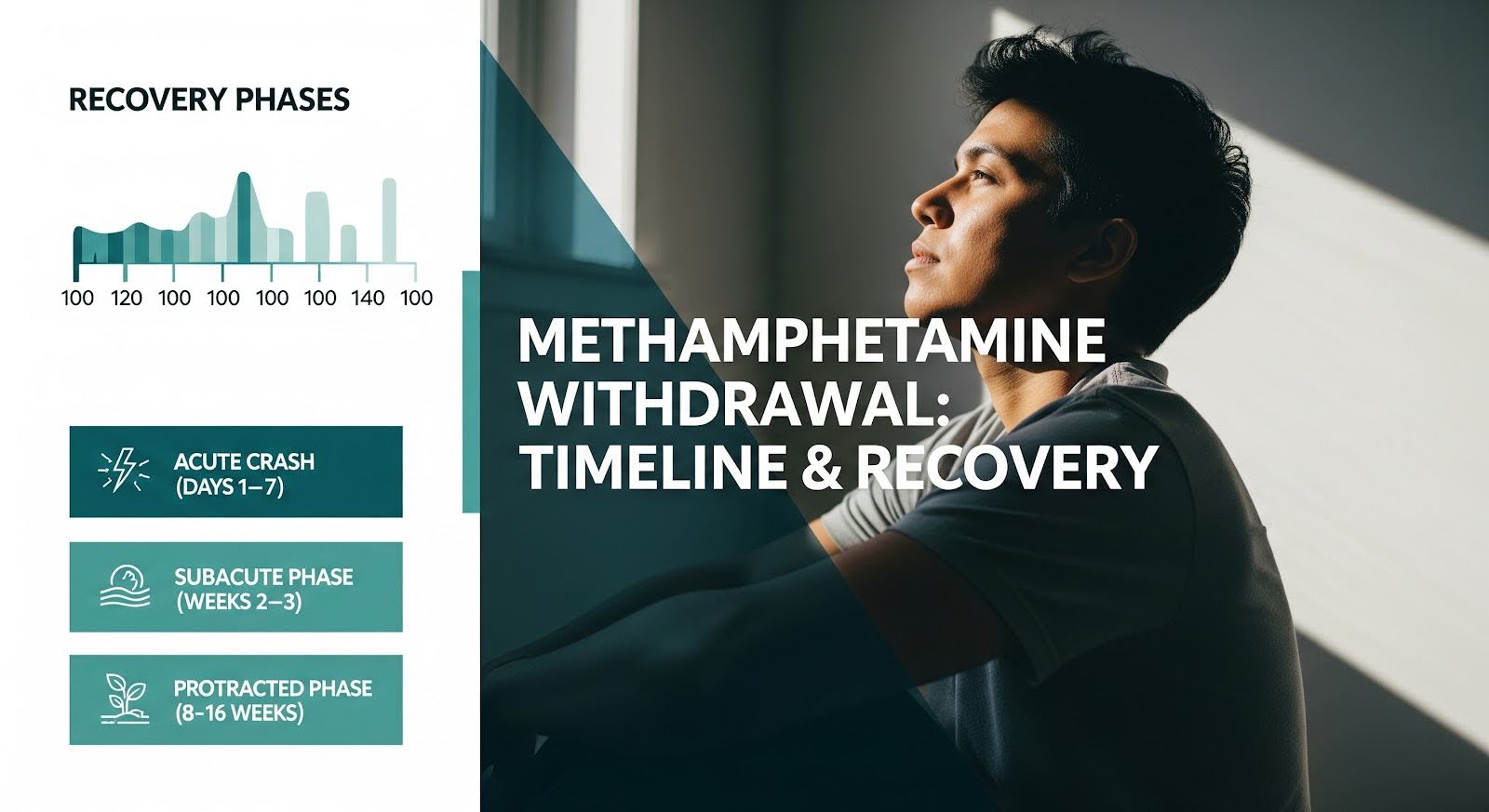
Withdrawal begins within 24 hours of last use and unfolds in distinct phases. The initial crash phase resolves in approximately one week, followed by subacute symptoms that can extend for 2 to 3 weeks. Some individuals experience protracted symptoms, including mood disturbances and cognitive deficits, that persist intermittently for 8 to 16 weeks.
Unlike alcohol withdrawal, which can cause delirium tremens with a measurable mortality risk of roughly 2% even with treatment, direct death from methamphetamine withdrawal alone appears rare. However, withdrawal is not benign.
The period carries indirect risks through suicidality, cardiovascular events in those with underlying heart disease, and polysubstance exposure, particularly fentanyl contamination in the current drug supply.
Common Meth Withdrawal Symptoms
Methamphetamine withdrawal produces a constellation of physical, emotional, and cognitive symptoms that vary in intensity depending on patterns of use, individual health, and co occurring conditions.
Early Crash Phase (Days 1 to 7)
The first week after stopping meth is marked by profound fatigue and a rebound effect as the brain adjusts to the absence of the drug. Common symptoms during this phase include:
- Hypersomnia or paradoxical insomnia
- Extreme fatigue and psychomotor slowing
- Depression, dysphoria, and anhedonia
- Irritability and anxiety
- Increased appetite (hyperphagia)
- Intense craving for methamphetamine
Some individuals experience transient psychotic features, particularly after heavy or chronic use, though frank psychosis is more typical of intoxication than uncomplicated withdrawal.
Subacute Phase (Weeks 2 to 3)
As the crash resolves, a second wave of symptoms emerges. These include:
- Persistent low mood and anxiety
- Sleep fragmentation and vivid dreams
- Cognitive deficits in attention, executive function, and memory
- Lingering low energy and motivation
- Continued craving
Protracted Symptoms (8 to 16 Weeks)
A subset of individuals experience extended symptoms that can last several months. These protracted symptoms are inconsistently measured across studies but are clinically important because they elevate relapse risk. They include:
- Recurrent anxiety or depression
- Sleep irregularities
- Heightened stress reactivity
- Cue driven craving triggered by people, places, or situations associated with past use
Women who use methamphetamine report more sleep problems than men and show stronger links between internalizing symptoms like anxiety and craving, suggesting that sex specific treatment approaches may improve outcomes.
Meth Withdrawal Timeline
Understanding the withdrawal timeline helps set realistic expectations and guides treatment planning.
| Phase | Time Window | Key Symptoms | Clinical Focus |
|---|---|---|---|
| Onset | Within 24 hours | Initial mood changes, fatigue, sleep disruption, craving | Safety assessment, hydration, suicide risk screening |
| Early Crash | Days 1 to 7 | Hypersomnia/insomnia, profound fatigue, depression, anxiety, increased appetite | Sleep support, mood stabilization, craving management, contingency management initiation |
| Subacute | Weeks 2 to 3+ | Persistent mood disturbance, sleep irregularities, cognitive slowing, low motivation | Behavioral therapies, relapse prevention, address co occurring disorders |
| Protracted | 8 to 16 weeks | Intermittent anxiety/depression, stress reactivity, cue induced craving | Long term relapse prevention, cognitive rehabilitation, ongoing support |
The acute detox period, when symptoms are most intense, typically spans 5 to 10 days. Functional symptoms commonly continue for 2 to 4 weeks.
Measurable neurobehavioral vulnerabilities can extend 6 to 12 months, requiring structured relapse prevention strategies even after classic vegetative symptoms fade.
How Long Does It Take to Detox from Meth?
The answer depends on how you define detox. If detox means the period of most intense physical and emotional discomfort, that window is roughly one week. If it means the time needed for major functional stabilization, plan for up to one month.
For full neurobehavioral recovery, including restoration of cognitive function and stress resilience, the process can take 6 to 12 months.
Symptom intensity and duration vary widely based on dose, frequency, route of use (smoking or injection versus oral), binge patterns, sleep debt, psychiatric comorbidities, and polysubstance exposure.
Heavy, high frequency use with smoking or injection typically produces more severe and prolonged withdrawal than lighter, less frequent use.
The drug supply itself has changed. Since 2011, U.S. methamphetamine seizures have reached historically high purity, often exceeding 90%, which may intensify acute withdrawal and craving.
Additionally, fentanyl co occurrence with methamphetamine, while nationally low at roughly 1%, exceeds 10% in several Northeastern states, creating geographically concentrated contamination risks that necessitate universal opioid screening and naloxone distribution during detox.

Meth Withdrawal Death Rate
Direct mortality attributable solely to methamphetamine withdrawal is likely rare compared to alcohol withdrawal delirium, which carries a 2% death rate with treatment and up to 25% without. However, the withdrawal period is not without serious risks.
Indirect Risks During Withdrawal
The highest near term dangers during meth detox stem from:
- Suicidality: Severe depression, anhedonia, and anxiety peak in the crash and subacute periods. Lack of longitudinal tracking in clinical trials should not be interpreted as absence of risk. Vigilant screening and safety planning are essential.
- Cardiovascular complications: National surveillance data show that stimulant involved overdose deaths without opioids more frequently involve documented cardiovascular disease (38.7% versus 21.2% in stimulant–opioid co involved deaths). Individuals with underlying heart conditions face elevated risk during withdrawal, particularly when agitation, insomnia, and anxiety trigger sympathetic surges.
- Polysubstance exposure: Between January 2021 and June 2024, 59% of overdose deaths involved stimulants, with 31% involving methamphetamine. Many of these deaths also involved opioids, especially fentanyl. During early abstinence, individuals may relapse or substitute substances, shifting acute overdose risk.
- Environmental hazards: Dehydration, poor nutrition, unsafe living conditions, and sleep deprivation compound withdrawal risks, especially for those experiencing homelessness or domestic violence.
Atlanta and Georgia Context
While specific methamphetamine withdrawal death rates for metro Atlanta are not readily available in public facing dashboards, Georgia’s surveillance infrastructure tracks substance related outcomes.
Analysts seeking county level emergency department and hospital discharge statistics on stimulant withdrawal in Fulton, DeKalb, and neighboring counties should use ICD 10 CM codes F15.23 (other stimulant dependence with withdrawal) and F15.93 (other stimulant use, unspecified with withdrawal) in Georgia Department of Public Health OASIS interfaces and apply CDC ESSENCE compatible query logic to generate reliable burden estimates.
Managing Meth Withdrawal Safely
There is no FDA approved medication specifically for methamphetamine withdrawal, but a combination of behavioral interventions, supportive care, and selective pharmacotherapy can ease symptoms and reduce relapse risk.
Behavioral Interventions
Contingency management has the strongest evidence base among behavioral treatments for stimulant use disorders.
This approach provides immediate, tangible rewards (such as vouchers or prizes) for objective evidence of abstinence, typically confirmed through urine drug screens.
A real world analysis of Veterans with stimulant use disorder found that contingency management exposure was associated with a 41% lower risk of death at one year, a clinically significant mortality benefit that justifies prioritizing access in detox and continuing care pathways.
Cognitive behavioral therapy and the Matrix Model, which combines CBT, relapse prevention, family education, and social support, are effective as standalone or adjunct therapies.
These approaches enhance coping skills and address the cognitive and emotional drivers of relapse.
Pharmacotherapy
No single medication has proven universally effective for methamphetamine withdrawal, but several agents show modest, phase dependent benefits:
- Mirtazapine: May help with severe insomnia and anxiety during the acute phase, though evidence is mixed. Use cautiously and only when opioid exposure is ruled out.
- Bupropion: A 300 mg per day sustained release formulation showed a trend toward reduced methamphetamine use in one trial, with significant benefit in men with low to moderate baseline use. It may help attenuate dysphoria and craving in early abstinence, particularly when combined with contingency management or CBT.
- Naltrexone: In combination with bupropion, naltrexone demonstrated efficacy for methamphetamine use disorder in a phase III trial. While not tested as a withdrawal treatment per se, it may support early recovery and relapse prevention, especially in patients with co occurring alcohol use.
- Modafinil: Mixed results, with some signals of symptom relief during inpatient withdrawal but no clear abstinence efficacy.
Pharmacotherapy should be individualized, time limited, and closely monitored, particularly in polysubstance contexts where drug interactions and side effects can complicate care.
Supportive Care and Harm Reduction
Practical detox components include:
- Suicide risk screening and safety planning
- Blood pressure and heart rate monitoring, especially in those with cardiovascular disease
- Sleep hygiene and nutrition support
- Naloxone distribution and education about fentanyl contamination risks
- Hydration and treatment of dehydration or malnutrition
- Warm handoffs to outpatient contingency management, CBT, peer recovery coaching, and co occurring disorder care
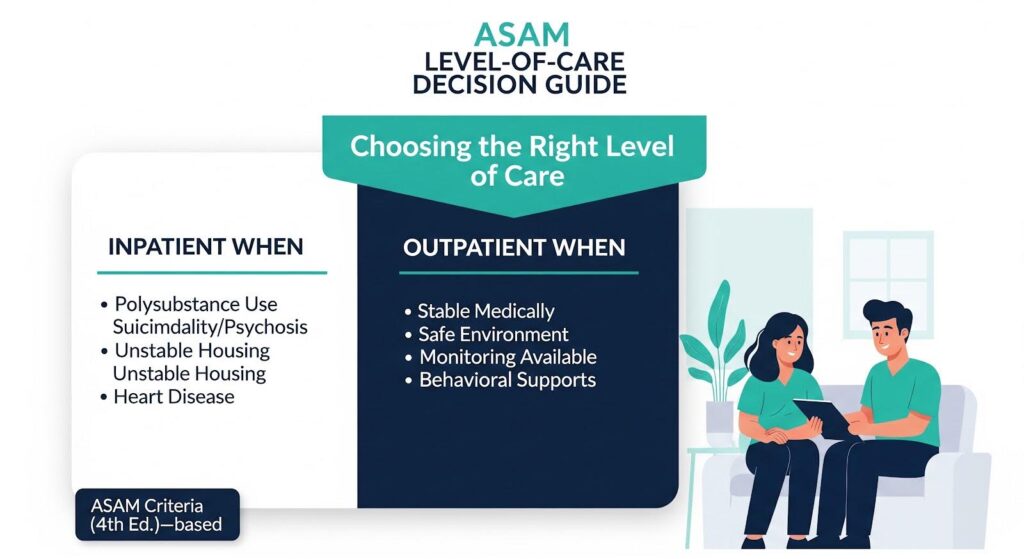
Choosing the Right Level of Care
Not everyone needs inpatient detox. The American Society of Addiction Medicine Criteria, Fourth Edition, provides a structured, dimension based framework to match individuals with the appropriate level of care based on withdrawal risk, biomedical and psychiatric comorbidities, relapse potential, and recovery environment.
Inpatient withdrawal management may be safer for individuals with:
- Severe polysubstance use, particularly involving opioids or benzodiazepines
- Acute psychiatric symptoms, including suicidality or psychosis
- Unstable or harmful social circumstances, such as homelessness or domestic violence
- Significant cardiovascular disease
Many others can be managed safely in outpatient settings with appropriate monitoring, crisis planning, phone or video check ins, and rapid linkage to behavioral supports like contingency management.
Why Detox is Just the Beginning?
Detox stabilizes the body and brain, but it does not address the underlying drivers of methamphetamine use disorder.
The protracted phase, lasting 6 to 12 months, is marked by cognitive inefficiency, anhedonia, stress reactivity, and episodic craving. These vulnerabilities are clinically meaningful and sustain relapse risk well beyond the resolution of acute symptoms.
Effective recovery requires a continuum of care that spans acute stabilization in the first week, functional recovery consolidation over 2 to 4 weeks, and structured relapse prevention and cognitive rehabilitation for at least 6 to 12 months.
Programs should incorporate phase specific supports, vigilantly screen for opioid exposure, deploy contingency management, and consider selective pharmacotherapeutic adjuncts where indicated.
If you or someone you care about is facing methamphetamine withdrawal, know that safe, compassionate support is available.
Thoroughbred Wellness & Recovery in Marietta offers evidence based medical detox with personalized care designed to guide you toward lasting freedom.