Mirtazapine and Buspirone: Can You Take Them Together?
Many people with depression and anxiety wonder if combining mirtazapine and buspirone is safe.
The FDA warns that mirtazapine can cause serotonin syndrome when taken with other serotonergic drugs, including buspirone, though serious reactions remain rare with careful monitoring.
This article explains the risks, when doctors prescribe both medications together, and how to stay safe if you’re considering this combination.
Understanding Mirtazapine and Buspirone
Mirtazapine is an antidepressant that works differently from common SSRIs. It blocks certain brain receptors to increase norepinephrine and serotonin while also blocking histamine receptors, which often causes sedation and increased appetite.
Doctors typically prescribe it for major depression, especially when patients struggle with insomnia or weight loss.
Buspirone is an anti-anxiety medication that acts as a partial agonist at serotonin 5-HT1A receptors.
Unlike benzodiazepines, it doesn’t cause sedation or carry addiction risk. Doctors use it for generalized anxiety disorder and sometimes add it to antidepressants when anxiety symptoms persist.
Both medications affect serotonin pathways in the brain, which raises questions about safety when used together.
What the FDA Says About This Combination?
The official FDA labeling for mirtazapine explicitly lists buspirone among medications that can increase the risk of serotonin syndrome.
This warning appears in the prescribing information for mirtazapine tablets, directing doctors to educate patients about symptoms and monitor closely during treatment initiation and dose changes.
The Mayo Clinic takes a conservative stance, advising patients not to use mirtazapine concurrently with buspirone due to serotonin syndrome risk. This reflects the medical community’s caution about combining serotonergic medications.
However, regulatory warnings don’t mean the combination is absolutely prohibited. They signal that doctors must weigh risks and benefits carefully, use lower doses, and monitor patients closely if they choose to prescribe both medications.
Serotonin Syndrome: What You Need to Know?
Serotonin syndrome is a potentially serious condition caused by too much serotonin activity in the brain.
Symptoms include agitation, confusion, rapid heart rate, high blood pressure, dilated pupils, muscle rigidity, tremor, sweating, diarrhea, and in severe cases, high fever and seizures.
The Hunter Serotonin Toxicity Criteria help doctors diagnose this condition. Key warning signs include spontaneous muscle twitching, muscle rigidity with fever, or tremor combined with overactive reflexes when taking serotonergic medications.
Research shows that serotonin syndrome risk increases most dramatically when different types of serotonergic drugs are combined, particularly MAOIs with SSRIs or SNRIs.
A large study of patients taking linezolid with antidepressants found that clinically significant serotonin syndrome occurred in less than 0.5% of cases, suggesting the overall risk remains low with careful patient selection and monitoring.
For the mirtazapine and buspirone combination specifically, the theoretical risk exists because both affect serotonin pathways.
Yet neither drug strongly increases serotonin levels the way SSRIs or MAOIs do, which may explain why severe reactions appear uncommon in clinical practice.
Real-World Safety Data
Pharmacovigilance databases track adverse events reported to the FDA. A comprehensive analysis of elderly patients found strong serotonin syndrome signals with SSRIs and MAOIs, with risk amplified by multiple serotonergic medications.
Older adults showed higher rates of reported serotonin toxicity, likely due to age-related changes in drug metabolism and common polypharmacy.
A separate analysis of mirtazapine adverse events from 2004 to 2024 identified nervous system disorders as the strongest safety signal. Many adverse events occurred within the first month of starting mirtazapine, highlighting the importance of early monitoring.
These databases cannot prove causation or provide exact risk percentages because reporting is voluntary and incomplete. However, they help identify patterns that inform safer prescribing practices.
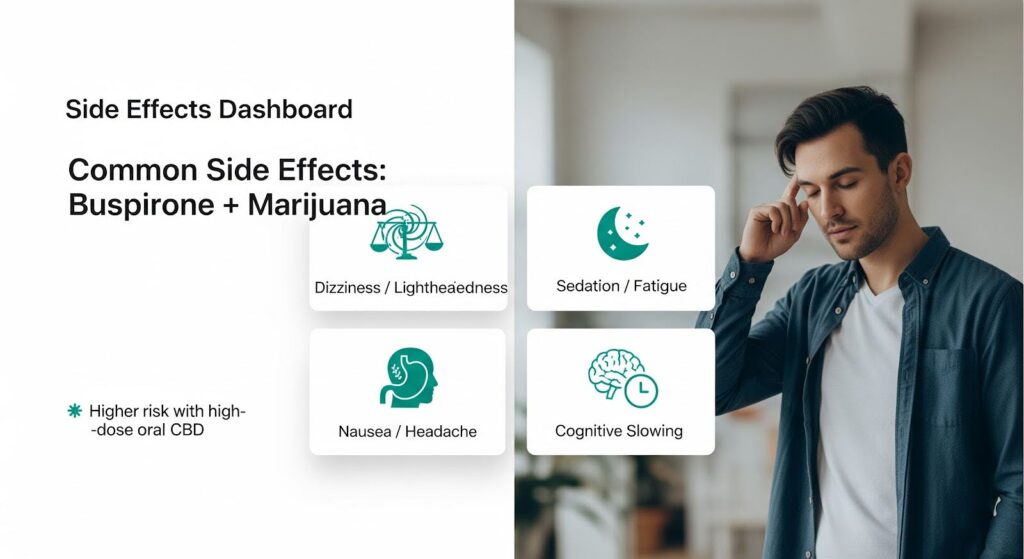
Common Side Effects When Taking Both Medications
When mirtazapine and buspirone are prescribed together, patients most often report:
- Excessive sedation and fatigue: Mirtazapine’s antihistamine effects cause drowsiness, which can worsen when combined with buspirone’s mild sedating properties
- Dizziness and lightheadedness: Both medications can cause these symptoms, especially during the first few weeks
- Dry mouth: Common with mirtazapine due to anticholinergic-like effects
- Increased appetite and weight gain: A hallmark of mirtazapine that some patients welcome but others find problematic
- Nausea and headache: Typical buspirone side effects that often improve with time
- Gastrointestinal upset: Including changes in bowel habits and abdominal discomfort
Most of these effects are manageable and don’t require stopping treatment. Taking mirtazapine at bedtime can turn sedation into a benefit for sleep, while taking buspirone with food may reduce nausea.
When Doctors Prescribe Both Medications?
Despite the warnings, some clinical situations may justify using mirtazapine and buspirone together:
Depression with insomnia and daytime anxiety: When a patient needs help sleeping and gaining appetite from mirtazapine but still experiences daytime anxiety, buspirone may address the residual anxiety without adding sedation.
SSRI or SNRI intolerance: Patients who cannot tolerate common antidepressants due to sexual side effects or gastrointestinal problems may benefit from mirtazapine for depression. If anxiety persists and benzodiazepines aren’t appropriate, buspirone becomes an option.
Treatment-resistant cases: When standard approaches haven’t worked, doctors sometimes carefully combine medications to target different symptom clusters.
The VA/DoD guidelines for depression note that no single antidepressant proves superior for initial treatment, emphasizing individualized selection based on patient factors.
This principle extends to combination strategies, which should be tailored to specific needs rather than used routinely.

Safety Guidelines for Combined Use
If your doctor prescribes both mirtazapine and buspirone, these precautions can minimize risk:
Before Starting Treatment
Review all your medications with your doctor, including over-the-counter drugs and supplements. Certain combinations are absolutely contraindicated:
- MAOIs (phenelzine, tranylcypromine, selegiline) require a 14-day washout period before starting mirtazapine
- Linezolid and methylene blue (antibiotics with MAOI properties) should not be combined with mirtazapine
- Other serotonergic medications (SSRIs, SNRIs, tramadol, triptans, St. John’s Wort) increase risk when added to the combination
Inform your doctor about liver or kidney problems, as mirtazapine clearance decreases with organ impairment, potentially requiring dose adjustments.
During Treatment
The NICE guidelines for depression recommend reviewing treatment within two to four weeks of starting or changing antidepressants.
This early check-in allows your doctor to assess effectiveness, monitor side effects, and adjust the plan before problems escalate.
Start with low doses of both medications. A typical approach might begin mirtazapine at 7.5 to 15 mg at bedtime and buspirone at 5 mg twice daily, then increase gradually based on response and tolerability.
Watch for warning signs of serotonin syndrome:
- New or worsening agitation, confusion, or restlessness
- Muscle twitching, rigidity, or tremor
- Rapid heartbeat or blood pressure changes
- Profuse sweating or shivering
- Diarrhea
- Fever
If you experience these symptoms, especially in combination, stop both medications immediately and seek urgent medical care.
Medication Interactions to Avoid
Certain drugs can increase mirtazapine levels in your blood, raising toxicity risk:
- CYP3A4 inhibitors like itraconazole, ritonavir, and nefazodone slow mirtazapine breakdown
- CYP3A4 inducers like phenytoin, carbamazepine, and rifampin speed up mirtazapine breakdown, potentially reducing effectiveness
Discuss any new prescriptions with your doctor to check for interactions.
Special Populations
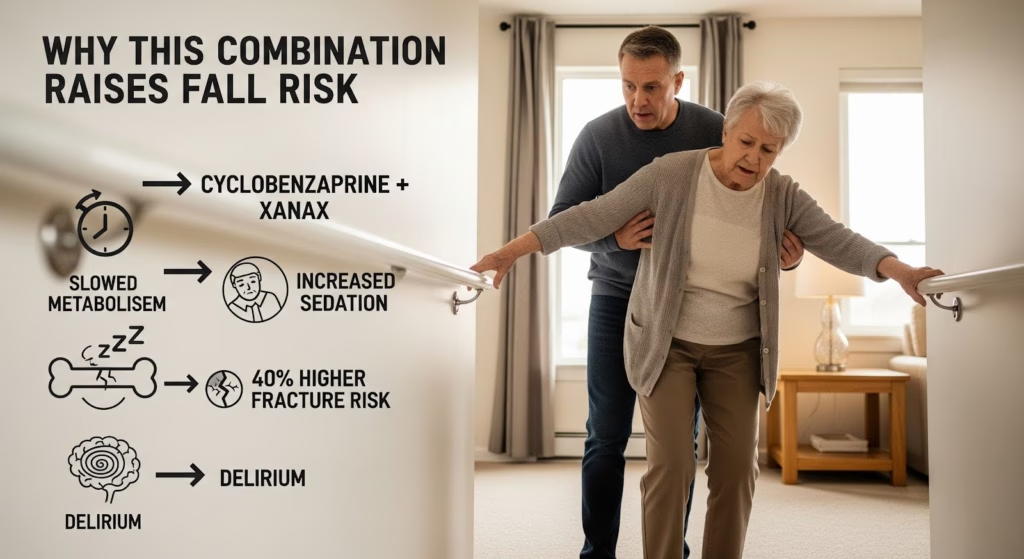
Older Adults
Elderly patients face higher serotonin syndrome risk due to age-related changes in drug metabolism and common use of multiple medications.
The pharmacovigilance analysis of elderly patients found stronger safety signals for serotonin toxicity in this age group.
If you’re over 65, your doctor should use the lowest effective doses, monitor more frequently, and minimize other serotonergic medications.
Falls risk also increases with sedation and dizziness, making careful dose titration essential.
Pregnancy and Breastfeeding
Mirtazapine is sometimes used during pregnancy for depression or severe nausea.
MotherToBaby reports that babies exposed in the womb may experience temporary symptoms like jitteriness, rapid heartbeat, or temperature regulation issues after birth, though these typically resolve quickly.
Small amounts of mirtazapine pass into breast milk, and most infants tolerate this without problems. However, excessive sleepiness in a breastfed baby warrants evaluation.
Buspirone has limited pregnancy safety data, making risk-benefit assessment crucial. Combining both medications during pregnancy should only occur when benefits clearly outweigh risks, with close coordination between your psychiatrist and obstetrician.
Liver or Kidney Disease
Mirtazapine clearance decreases in moderate to severe liver or kidney impairment. If you have organ dysfunction, your doctor may prescribe lower doses and monitor more carefully for side effects.
Alternatives to Consider
Before combining mirtazapine and buspirone, consider these options:
Psychotherapy: Cognitive behavioral therapy and other evidence-based therapies can treat depression and anxiety without medication interactions. The VA/DoD guidelines recommend either psychotherapy or medication as appropriate first-line treatments.
Monotherapy optimization: Increasing the dose of one medication or switching to a different antidepressant may address both depression and anxiety without adding a second drug.
Different combinations: If augmentation is needed, other strategies like adding psychotherapy, switching antidepressants, or using different medication combinations may carry less interaction risk.
The NICE guidance on anxiety disorders emphasizes treating the primary condition first. If depression and anxiety coexist, treating depression often improves anxiety symptoms as well.
Making an Informed Decision
The combination of mirtazapine and buspirone is not categorically unsafe, but it requires careful consideration and monitoring. The FDA warning reflects real risk, even if serious reactions remain uncommon.
This combination makes most sense when:
- You have a clear reason that justifies using both medications
- You cannot tolerate or haven’t responded to safer alternatives
- You can commit to close monitoring and early follow-up
- You understand the warning signs of serotonin syndrome
- Your medication list is free of other high-risk serotonergic drugs
The combination is generally inappropriate when:
- You’re taking MAOIs or other strong serotonergic medications
- You’re elderly with multiple medications
- You have significant liver or kidney disease without capacity for close monitoring
- Safer alternatives haven’t been tried
What to Discuss With Your Doctor?
Before starting this combination, have an open conversation about:
- Why both medications are necessary for your specific situation
- What alternatives exist and why they may not be suitable
- The specific risks based on your age, health conditions, and other medications
- The monitoring plan, including when you’ll be seen for follow-up
- Warning signs that should prompt you to stop the medications and seek care
- How long you’ll likely need both medications
Document this discussion and the agreed-upon plan. The NICE depression guidelines emphasize creating an explicit management plan covering initial doses, expected benefits, potential side effects, and withdrawal effects.
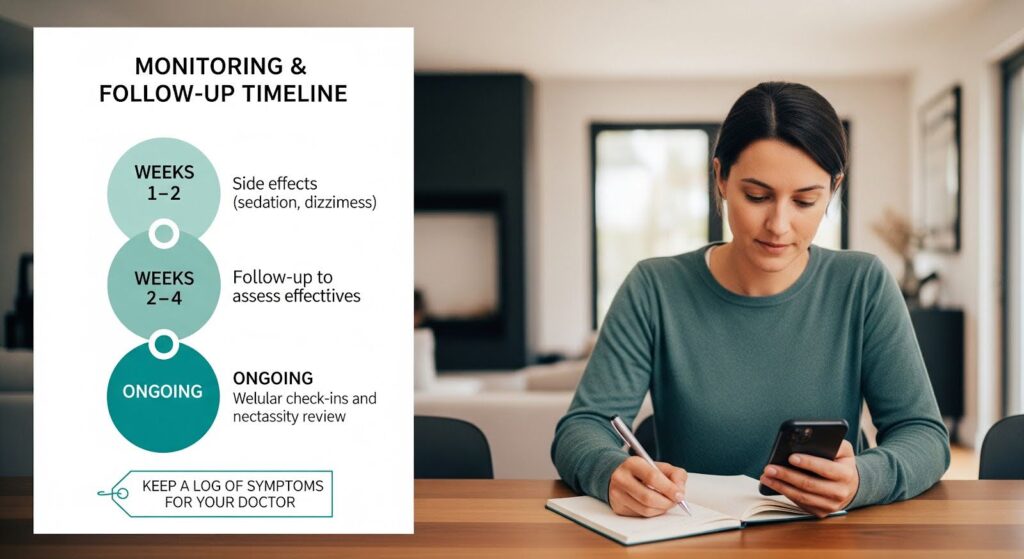
Monitoring and Follow-Up
If you start both medications, expect:
- Week 1-2: Close attention to sedation, dizziness, and early side effects; contact your doctor if symptoms are severe or concerning
- Week 2-4: Scheduled follow-up to assess effectiveness, side effects, adherence, and any new medications or supplements
- Ongoing: Regular check-ins to evaluate whether both medications remain necessary and beneficial
Keep a simple log of your symptoms, side effects, and any changes in other medications. This helps your doctor make informed adjustments.
When to Seek Immediate Help?
Stop both medications and seek emergency care if you experience:
- Severe agitation, confusion, or hallucinations
- Muscle rigidity or uncontrollable muscle twitching
- High fever (over 101°F or 38.3°C)
- Rapid or irregular heartbeat
- Seizures
- Loss of consciousness
These symptoms may indicate serotonin syndrome or another serious reaction requiring immediate medical attention.
For less urgent but concerning symptoms like persistent dizziness, excessive sedation interfering with daily activities, or troublesome side effects, contact your doctor promptly for guidance.
The Bottom Line
Taking mirtazapine and buspirone together is possible but requires careful medical supervision.
The FDA explicitly warns about serotonin syndrome risk with this combination, and safety data from thousands of patients show that older adults and those on multiple medications face higher risk.
Most patients who take both medications experience manageable side effects like sedation, dizziness, and appetite changes rather than serious toxicity.
However, the potential for serotonin syndrome means this combination should be reserved for situations where benefits clearly justify the risks and safer alternatives have been considered.
If your doctor recommends both medications, make sure you understand why, know the warning signs to watch for, and commit to early follow-up.
Start with low doses, avoid other serotonergic drugs when possible, and maintain open communication about how you’re feeling.
Depression and anxiety deserve effective treatment, but safety must come first. With proper precautions and monitoring, many patients can benefit from this combination when it’s truly needed.
If you’re struggling with co-occurring depression and anxiety and want expert guidance on the safest, most effective treatment approach for your unique situation, reach out to our team for a confidential consultation.